Emergency care and nursing in case of Hypertensive crisis
Affecting one quarter of the adult
population (60 million in the United States and 1 billion people worldwide),
arterial hypertension is the leading cause of death in the world and the most
common cause for an outpatient visit to a physician; it is the most easily
recognized treatable risk factor for stroke, myocardial infarction, heart
failure, peripheral vascular disease, aortic dissection, atrial fibrillation,
and end-stage kidney disease. Despite this knowledge and unequivocal scientific
proof that treatment of hypertension can prevent many of its life-altering
complications, hypertension remains untreated or undertreated in the majority
of affected individuals in all countries, including those with the most
advanced systems of medical care. Inadequate treatment of hypertension is a
major factor contributing to some of the adverse secular trends since the early
1990s, including an increased incidence of stroke, heart failure, and kidney
failure plus a leveling off of the decline in coronary heart disease mortality.
Across populations, the risks of
heart disease and stroke increase continuously and logarithmically with
increasing levels of systolic and diastolic blood pressure at or above 115/75
mm Hg . Thus, the dichotomous separation of “normal”
from “high” blood pressure is artificial, and the definition of arterial
hypertension (i.e., high blood pressure) has been a moving target. On the basis
of results of randomized clinical drug trials, hypertension currently is
defined as a usual blood pressure of 140/90 mm Hg or higher, the value above
which the benefits of treatment appear to outweigh the risks. Prehypertension
is a new designation for mildly elevated blood pressures between 120/80 and
139/89 mm Hg, a level at which progression to hypertension is twice as likely
as with a blood pressure below 120/80 mm Hg, and cardiovascular risk retains
its continuous log-linear function compared with lower blood pressures. The cardiovascular
mortality rate is only half as great at 120/80 mm Hg as at 140/90 mm Hg, but it
is unknown whether the benefits of treating prehypertension outweigh the risks.
Arterial hypertension, defined as a
systolic blood pressure (SBP) in excess of 140 mm Hg and/or diastolic
blood pressure (DBP) in excess of 90
mm Hg, has long been identified as an independent risk
factor for cardiovascular disease. Traditionally, emphasis has been placed on
elevated DBP as a risk factor for the development of target organ damage.
However, as early as 1971, the Framingham study showed that, although DBP was a
major determinant of cardiovascular risk in men under 45 years of age, SBP was
the stronger risk factor in older men and in women of all ages.
Since then, several observational studies have suggested that the pulse
pressure (PP) may be a better predictor of cardiovascular complications than
SBP or mean arterial pressure.
Data from the National Health and
Nutrition Examination Survey has demonstrated that if a blood pressure (BP) of
140/90 mm Hg is considered to be normal, only 27% of hypertensive patients are
adequately controlled in the United
States. Recommendations from the Joint
National Committee on the Prevention, Detection, Evaluation and treatment of
High Blood Pressure (JNC-VI report) now regard a BP of 140/90 mm Hg as high
normal and 130/85 mm Hg as normal. For
diabetic patients, therefore, it is recommended that BP be reduced below 130/85
mm Hg and for those with renal impairment, evidenced by proteinuria,
pressures should be reduced below 125/75 mm Hg. In patients with underlying
coronary artery disease, the BP should be reduced below 120/80 mm Hg.
The beating heart generates pressure
and flow waves which propagate throughout the arterial system. The shape of the
pressure and flow waves is altered by their continuous interaction with the
non-uniform arterial system. The pressure and flow waves can be studied in
terms of a forward component, running from the heart itself, and a backward
component carrying information on the peripheral arterial system.
In the presence of arteriosclerosis
and aortic stiffening (consequences of arterial hypertension), the pulse wave
velocity is increased, causing the pulse waves to reflect more quickly off the
arteriolar vessels and return to the large vessels during systole. This
amplifies SBP. In the presence of normal vascular compliance, the reflected
waves return during diastole and augment DBP. Consequently, arteriosclerosis
tends simultaneously to increase SBP and decrease DBP, resulting in a widened
pulse pressure.
A widened pulse pressure increases
cardiovascular morbidity because elevated SBP is associated with greater left
ventricular workload and myocardial oxygen demand, whereas a decreased DBP may
decrease coronary perfusion, resulting in decreased myocardial oxygen supply
and a greater risk for myocardial ischemia and injury.
Hypertension (systolic pressure  140 mm Hg or
diastolic pressure
140 mm Hg or
diastolic pressure  90 mm Hg) is present in one in four adults in the United
States.1 The prevalence is higher among blacks
and older persons, especially older women. Table 1 shows the classification of
blood pressure according to the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.2 Hypertension is a risk
factor for stroke, myocardial infarction, renal failure, congestive
heart failure, progressive atherosclerosis, and dementia.3 Systolic pressure
is a stronger predictor of
cardiovascular events than is diastolic pressure,4 and isolated systolic hypertension, which
is common among older persons, is particularly hazardous.5 There is a continuous, graded relation between blood
pressure and the risk of
cardiovascular disease; the level and duration of hypertension and the presence or absence of coexisting cardiovascular risk
factors determine the outcome.6 Treatment of hypertension reduces the risk of stroke, coronary artery disease, and congestive
heart failure, as well as overall cardiovascular morbidity and mortality
from cardiovascular causes. However, only 54 percent of patients with hypertension receive treatment and only 28 percent
have adequately controlled blood pressure.1
90 mm Hg) is present in one in four adults in the United
States.1 The prevalence is higher among blacks
and older persons, especially older women. Table 1 shows the classification of
blood pressure according to the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.2 Hypertension is a risk
factor for stroke, myocardial infarction, renal failure, congestive
heart failure, progressive atherosclerosis, and dementia.3 Systolic pressure
is a stronger predictor of
cardiovascular events than is diastolic pressure,4 and isolated systolic hypertension, which
is common among older persons, is particularly hazardous.5 There is a continuous, graded relation between blood
pressure and the risk of
cardiovascular disease; the level and duration of hypertension and the presence or absence of coexisting cardiovascular risk
factors determine the outcome.6 Treatment of hypertension reduces the risk of stroke, coronary artery disease, and congestive
heart failure, as well as overall cardiovascular morbidity and mortality
from cardiovascular causes. However, only 54 percent of patients with hypertension receive treatment and only 28 percent
have adequately controlled blood pressure.1

Strategies and Evidence
Evaluation
Accurate measurement of
blood pressure7 and verification of elevated pressure on multiple occasions
over time are important. Ambulatory or home blood-pressure
monitoring8 can identify "white-coat hypertension" (blood pressure
that is elevated when measured during an office visit but that is otherwise
normal) and prevent unnecessary treatment. White-coat hypertension, present in 20 percent
of patients with
elevated blood pressure, is associated with a lower cardiovascular
risk than is sustained hypertension,
but it may be a precursor of
sustained hypertension
and therefore warrants monitoring.
In addition to the history taking and physical examination, several
tests are routinely indicated in patients with hypertension: urinalysis, complete blood
count, blood chemical tests (measurements of potassium, sodium, creatinine,
fasting glucose, total cholesterol, and high-density lipoprotein),
and 12-lead electrocardiography. The evaluation should identify
signs of
cardiovascular, cerebrovascular, or peripheral vascular disease and
other cardiovascular risk factors that are frequently present in
patients with hypertension.
Severe or resistant hypertension
or clinical or laboratory findings suggesting the presence of renal disease, adrenal hypertension (due to
abnormal mineralocorticoid secretion or pheochromocytoma), or
renovascular hypertension
should be further investigated. Essential, or primary, hypertension, the focus of this article, is the
diagnosis in over 90 percent of
cases.
Video:
hypertensive heart
Treatment
The primary goal of
the treatment of hypertension is to prevent cardiovascular
disease and death. Coexisting cardiovascular risk factors increase
the risks associated with hypertension
and warrant more aggressive treatment.
The five-year risk of
a major cardiovascular event in a 50-year-old man with a blood pressure
of 160/110 mm Hg is
2.5 to 5.0 percent; the risk doubles if the man has a high
cholesterol level and triples if he is also a smoker.9
The benefits of
lowering blood pressure, first demonstrated after short-term treatment of malignant hypertension,10 have subsequently been demonstrated in all
stages of hypertension. Trials
involving patients with stage 1 or 2 hypertension
showed that lowering systolic pressure by 10 to 12 mm Hg and diastolic pressure
by 5 to 6 mm
Hg reduces the risk of
stroke by 40 percent, the risk of coronary disease by 16 percent, and the risk of death from any
cardiovascular cause by 20 percent.11,12 The higher the blood pressure and the
number of risk
factors, the greater the reduction in absolute risk (and the smaller
the number needed to treat).
Determination of
the need for drug therapy is based on a combined assessment of the blood-pressure level and the
absolute risk of
cardiovascular disease (Figure 1). Patients with stage 1 hypertension can be treated with
lifestyle modifications alone for up to one year, if they have no
other risk factors, or for up to six months, if they have other risk
factors. Drug treatment
should be provided if blood pressure remains elevated after a
trial of lifestyle
modifications alone. Lifestyle modifications and antihypertensive
therapy are indicated for patients with cardiovascular or other
target-organ disease (renal, cardiac, cerebrovascular, or retinal
disease) and for those with stage 2 or 3 hypertension. Patients with diabetes
are at high risk, and drug therapy is indicated in such patients
even if blood pressure is at the high end of the normal range.

Figure 1. Treatment of Hypertension According to the Level of
Blood Pressure and Cardiovascular Risk.
Two or more blood-pressure
readings separated by two minutes should be averaged. If the pressure is at the
high end of the normal range, it should be rechecked yearly. Stage 1
hypertension should be confirmed within two months. Patients with stage 2
hypertension should be evaluated and referred for care within one month; those
with stage 3 hypertension should be evaluated immediately or within one week.
If systolic and diastolic values are in different categories, the
recommendations for the higher reading should be followed.
Laboratory tests include a
complete blood count; measurements of potassium, sodium, creatinine, fasting
glucose, total cholesterol, and high-density lipoprotein cholesterol; and
urinalysis. ECG denotes electrocardiography. Cardiovascular or other
target-organ disease denotes left ventricular hypertrophy, angina or prior
myocardial infarction, prior coronary revascularization, heart failure, stroke
or transient ischemic attack, nephropathy, peripheral arterial disease, and
retinopathy.
For patients with multiple
risk factors, clinicians should consider drugs as initial therapy along with
lifestyle modifications. Clinically important risk factors include smoking,
dyslipidemia, diabetes mellitus, an age of more than
60 years, male sex, postmenopausal status in women, and a family history of
cardiovascular disease for women under the age of 65 years and men under the
age of 55 years. Adapted from the Joint National Committee on Prevention,
Detection, Evaluation, and Treatment of High Blood Pressure.2
Lifestyle Modifications
Table 2 lists lifestyle modifications recommended for all patients with
hypertension. The
Dietary Approaches to Stop Hypertension
(DASH) study showed that eight weeks of a diet of
fruits, vegetables, low-fat dairy products, whole grains, poultry,
fish, and nuts, with limited fats, red meat, and sweets, reduced
systolic pressure by 11.4
mm Hg and diastolic pressure by 5.5 mm Hg.13 With sodium intake at a level below 100
mmol per day, systolic pressure was 3 mm Hg lower and diastolic
pressure was 1.6 mm
Hg lower than with the DASH diet and a higher level of sodium intake.14

Restriction of sodium intake to 2 g per day lowers systolic
pressure, on average, by 3.7 to 4.8 mm Hg and lowers diastolic pressure,
on average, by 0.9 to 2.5 mm
Hg,15,16 although the reductions
vary from person to person beyond these ranges. Salt sensitivity is
common in elderly patients with hypertension.
Despite concern that salt restriction for all patients with hypertension might have
adverse consequences,17 moderate sodium restriction appears to be
generally safe and effective18 and is particularly effective in elderly
persons.19
Whether lifestyle
modifications can be sustained is a concern. Four years after
enrollment in the Treatment
of Mild Hypertension Study,
patients with stage 1 hypertension
had gained back half the weight lost after one year of intervention and were less successful
at maintaining a low sodium intake and an increased level of physical activity than
they had been at one year.20 Nevertheless, lifestyle modifications
alone controlled blood pressure at four years in 59 percent of the patients.
Most clinical trials
of lifestyle modifications
have been underpowered or of
insufficient duration to evaluate the effect of these interventions on major
cardiovascular outcomes. However, lifestyle modifications should be
encouraged, since they are safe and inexpensive and, when combined with
drug therapy, may result in better blood pressure control and an
improved quality of
life.21
Treatment Goal for Blood
Pressure
The risk of cardiovascular disease remains
higher in treated patients with hypertension than in persons with normal blood pressure,
suggesting that treatment
targets have not been low enough. Greater reductions in blood
pressure have been shown to be safe and beneficial.22,23 In the Hypertension
Optimal Treatment
trial, the risk of
major cardiovascular events was lowest among patients whose blood
pressure had been reduced to 138.5/82.6 mm Hg. An additional
reduction did not further reduce the risk of events in nondiabetic patients,
but it was not harmful. Among diabetic patients, the lowest rates of major cardiovascular
events and death from cardiovascular causes were achieved with the
lowest blood pressure. In patients over the age of 65 years, morbidity and mortality
from cardiovascular disease are reduced when systolic pressure is
lowered to a level below 160 mm Hg.24 Whether levels below 140 mm Hg provide additional
protection is unclear.
Choice
of Antihypertensive
Drugs
Most
antihypertensive drugs reduce blood pressure by 10 to 15 percent.
Monotherapy is effective in about 50 percent of unselected patients, and those
with stage 2 or 3 hypertension
often need more
than one drug.25 There have been few comparative trials of antihypertensive agents
that have had sufficient power to demonstrate an advantage of one drug over another, and
there is individual variation in responsiveness to drugs. Thus, the
choice of therapy
is based on a combined assessment of
several characteristics of
the patient: coexisting conditions, age, race or ethnic group, and
the response to previously used drugs, including the presence or
absence of adverse
reactions.
A critical issue is
whether a drug reduces cardiovascular morbidity and mortality. As
compared with placebo, diuretics and beta-blockers reduce the risk of stroke, coronary heart disease,
and overall mortality from cardiovascular disease in unselected patients
with hypertension
who do not have preexisting coronary disease, diabetes, or
proteinuria.11,12 A meta-analysis of trials involving more than 26,000
patients showed that, as compared with placebo, angiotensin-converting–enzyme
(ACE) inhibitors reduce the risk of stroke, coronary heart disease, major
cardiovascular events, death from cardiovascular causes, and death
from any cause,26 although the results were heavily dependent on a
trial in which all the participants had preexisting cardiovascular
disease or diabetes and some did not have hypertension.27
Calcium-channel antagonists, as compared
with placebo, reduce the risk of
stroke, major cardiovascular events, and death from
cardiovascular causes; however, these drugs do not significantly
reduce the risk of
coronary heart disease, heart failure, or death from any cause.26
The question of whether antihypertensive agents
differ in their ability to prevent adverse outcomes has been
difficult to answer.28 Some data suggest potentially
important differences. For example, ACE inhibitors were more
effective than calcium-channel antagonists in preventing coronary
heart disease in one trial,29 but not in another, larger study.30 A meta-analysis of clinical trials suggests that ACE
inhibitors are more effective than calcium-channel antagonists in
reducing the risk of
heart failure but not in reducing the risk of stroke, death from cardiovascular
disease, or death from any cause.26 Losartan, an angiotensin-receptor antagonist,
has recently been shown to be more effective than atenolol in
reducing the risk of stroke.31 Another meta-analysis suggests that
calcium-channel antagonists may prevent stroke to a greater extent
than diuretics or beta-blockers but have not been shown to provide
similar protection against coronary heart disease.32 The Antihypertensive and
Lipid-Lowering Treatment
to Prevent Heart Attack Trial, the largest randomized trial comparing
several antihypertensive agents as initial
therapy, demonstrated that in patients older than 55 years (35
percent of
whom were black and 19 percent of
whom were Hispanic), diuretic-based therapy was as effective as treatment with calcium-channel
antagonists or ACE inhibitors in preventing major coronary events.33
Diuretic-based therapy was slightly
more effective than treatment
with calcium-channel antagonists in preventing heart failure and
was more effective than treatment
with ACE inhibitors in preventing stroke and heart failure. A
smaller study of elderly
white men and women with hypertension,
showed that ACE-inhibitor–based therapy was slightly more effective
than diuretic-based therapy in preventing myocardial infarction (only
in men) but not stroke.34
On the basis of the available data, diuretics or
beta-blockers remain appropriate for the initial treatment of uncomplicated hypertension, despite the concern that
these agents may be associated with adverse metabolic effects (e.g.,
hyperuricemia and impaired glucose tolerance). Alternative drugs are
preferable for patients with certain coexisting medical conditions (Table 3). In particular, ACE inhibitors and
angiotensin-receptor antagonists are appropriate initial therapy in patients with
diabetes mellitus, renal disease, or congestive heart failure35,36 (though beta-blockers and diuretics are
also useful in patients with heart failure); ACE inhibitors can also
be used in patients with prior myocardial infarction or coronary
artery disease. Short-acting calcium-channel antagonists cause a
rapid, acute drop in blood pressure, which may precipitate coronary
ischemia, and long-acting calcium-channel antagonists are therefore
preferred when this class of agent is chosen.37 Alpha-blockers relieve symptoms associated
with prostatic hypertrophy. Since they are not as effective as other
agents in reducing the risk of cardiovascular
disease, they should be used as second- or third-line therapy.33

Other
Considerations in the Choice of Therapy
Age and race have been shown
to be determinants of the response to specific antihypertensive
medications. The Department of Veterans Affairs Cooperative Study
reported that younger whites had a good response to ACE inhibitors
and beta-blockers, whereas older blacks had a better response to
diuretics or calcium-channel antagonists.25
Hypertension is more
severe and target-organ damage, particularly end-stage renal disease,
more prevalent among blacks. Salt sensitivity is common, and sodium
restriction should be encouraged. Although the magnitude of the
blood-pressure response to monotherapy with a diuretic or a
calcium-channel antagonist may be greater than the response to
monotherapy with another agent, significant reductions occur with
ACE inhibitors, angiotensin-receptor antagonists, and beta-blockers
when an adequate dose is given.38
Side effects differ according
to the class of antihypertensive drug (Table 3). Although
adverse effects are reported by 10 to 20 percent of patients taking
such drugs, the quality of life improves when hypertension is
treated.21
The Treatment of Mild Hypertension Study and the Department of
Veterans Affairs Cooperative Study both demonstrated that among the
five main classes of antihypertensive drugs (diuretics,
beta-blockers, calcium-channel antagonists, ACE inhibitors, and
alpha-blockers), no one drug is more acceptable than the others,
except that sexual dysfunction is more common among men treated with
the diuretic chlorthalidone.21,25
Use of lower-cost, generic drugs that require less frequent doses
can improve compliance.
Combination
Therapy
The use of lower doses of two
or more drugs with complementary mechanisms may lower blood pressure
with fewer adverse effects than the use of higher doses of a single
agent. Most combination therapies include small doses
of a diuretic, which potentiate the effects of other drugs (ACE
inhibitors, angiotensin-receptor antagonists, or beta-blockers).
Combination therapy may improve compliance and achieve the target
blood pressure more rapidly.
Guidelines
National and international
groups have issued guidelines for the treatment of hypertension. The
main differences among these guidelines are the criteria for
initiating drug therapy in low-risk patients with stage 1
hypertension. The Joint National Committee on Prevention, Detection,
Evaluation, and Treatment of High Blood Pressure2 and
the World Health Organization–International Society of Hypertension41
recommend stratification of patients into risk categories on the
basis of age, sex, smoking status, presence or absence of diabetes,
cholesterol level, presence or absence of preexisting cardiovascular
disease, and presence or absence of target-organ damage (Figure 1). Drug
treatment is recommended for stage 1 or higher hypertension if blood
pressure does not decrease after a certain period of
lifestyle-modification counseling (6 to 12 months, according to the
Joint National Committee guidelines). The British Hypertension
Society and New Zealand guidelines recommend the use of tables that
quantify a person's 5- or 10-year risk of a cardiovascular event;
drugs are recommended only if the 5-year risk is at least 10
percent.42,43 When
drugs are indicated, the guidelines recommend those that have been
shown to improve cardiovascular outcomes, with coexisting conditions
and demographic characteristics taken into account.
Areas of Uncertainty
Although moderate sodium
restriction lowers blood pressure, the small effects, variability in
response, and lack of a proven cardiovascular benefit have led to
uncertainty about whether it should be broadly recommended. There is
also uncertainty about whether specific properties of certain drugs
result in differential effects on morbidity and mortality that are
independent of the reduction in blood pressure.
The use of drugs in patients
with a low absolute risk of cardiovascular disease is controversial.
The rationale for withholding drugs from such patients is that some
trials have shown that mortality among low-risk patients treated
with drugs is similar to that in control groups.44
However, given that even high-normal blood pressures (130 to 139/85
to 89 mm
Hg) are associated with an increased risk of cardiovascular disease,45
there is concern about withholding drugs from "low-risk"
patients. Also, the feasibility of basing treatment decisions on the
use of tables for calculating the absolute risk of cardiovascular
disease has not been assessed.
The appropriate strategy for
choosing the initial antihypertensive therapy is still unresolved. Some
have proposed that the choice of treatment should be based on renin
levels,46
but this approach is not widely used. Whether combination therapy as
the initial treatment leads to better control of blood pressure and
a lower risk of cardiovascular disease than monotherapy is also
unresolved. Finally, optimal blood-pressure targets remain to be
determined, particularly for elderly patients.
Conclusions and
Recommendations
Hypertension affects 25
percent of adults in the United
States and is adequately treated
in less than 30 percent of them. Appropriate therapy can reduce
blood pressure and cardiovascular morbidity and mortality.
Persons who have stage 1
hypertension and are at low risk for cardiovascular disease can be
treated with lifestyle modifications for up to one year.
Patients who have stage 1 hypertension and other cardiovascular risk
factors or a higher stage of hypertension should be treated with drugs to reduce blood pressure to a level below 140/90
mm Hg, or to reduce pressure to 130/80 mm Hg or less if the patient
has diabetes, renal disease, or both.
Diuretics and
beta-blockers are appropriate as first-line therapy for patients without
coexisting conditions. ACE
inhibitors or angiotensin-receptor antagonists are recommended for
patients with type 2 diabetes, kidney disease, or both and are also
useful in patients with heart failure. Beta-blockers and ACE
inhibitors are recommended in patients with prior myocardial
infarction, and calcium-channel antagonists benefit elderly patients
at risk for stroke. If blood pressure is not controlled with an
optimal dose of a single drug, a second agent with a complementary mechanism
of action should be added. Combination therapy provides more rapid
control of blood pressure than does
monotherapy and is therefore an initial treatment option for
patients with stage 2 or 3 hypertension.
Resistant or Difficult-to-Control Hypertension
Case vignette. A 70-year-old woman
with a long-standing history
of hypertension comes
for follow-up. Her
medications include atenolol (100 mg daily), hydrochlorothiazide (12.5 mg daily),
lisinopril (40 mg daily), and ibuprofen (400 mg twice daily for osteoarthritis). She
does not smoke or
drink alcohol. Her body-mass index (the weight in kilograms divided
by the square of the height in meters) is 32. Her systolic and diastolic blood pressures (measured
three times while she was seated) range from 164 to 170 mm Hg and 92 to 96 mm Hg, respectively, and
the pulse rate is 72 per minute. Examination of her ocular fundi
reveals arteriolar narrowing. The results of cardiovascular
examination are normal.
There are no abdominal bruits. The serum potassium level is 3.8 meq
per liter, and the serum creatinine level is 1.2 mg per deciliter (106
µmol per liter); there is no microalbuminuria. How should this patient
be further evaluated and treated?
The Clinical Problem
Resistant, or
refractory, hypertension is defined by a blood
pressure of at least 140/90 mm Hg or
at least 130/80 mm Hg in patients with diabetes or renal disease (i.e., with a
creatinine level of more
than 1.5 mg per deciliter [133 µmol per liter] or urinary protein excretion of more than 300 mg over a
24-hour period), despite adherence to
treatment with full doses of at least three antihypertensive
medications, including a diuretic. Patients who have recently
received a diagnosis of hypertension
or who have not yet
received treatment should not be considered to have resistant hypertension, regardless of
their blood-pressure level.
Data on the
prevalence of resistant
hypertension are
scant. In large clinical trials of hypertension in which protocols required drug
titration until the blood pressure was below a predefined target,
the diastolic blood
pressure was below 90 mm
Hg in approximately 90 percent of patients, but the systolic blood pressure was
below 140 mm
Hg in only 60 percent of patients. However, patients who had no
predefined response to
treatment did not meet all of the criteria for resistant hypertension
as cited above. In one specialty hypertension
clinic, only 59 percent of patients whose hypertension was considered to be resistant had blood pressures below
140/90 mm Hg despite careful drug titration. These observations
suggest that blood-pressure goals may be difficult to achieve in as many as 40 percent
of patients. Resistant
or difficult-to-control systolic
hypertension is
more common in
patients over the age of 60 years than in younger patients.
Patients whose hypertension is uncontrolled are more likely to have target-organ damage and a higher long-term
cardiovascular risk than are patients whose blood pressure is controlled. Heart
failure, stroke, myocardial infarction, and renal failure are
related to the degree
of the elevation in blood pressure. Other risk factors, such as diabetes and
dyslipidemia, further increase the cardiovascular risk in these
patients.
Difficult-to-control hypertension is
defined here as persistently elevated blood pressure despite treatment
with two or three
drugs but not meeting the above-mentioned strict criteria for resistant hypertension.
Difficult-to-control hypertension is far more common than resistant
hypertension.
Strategies and Evidence
Formal studies of the management of resistant or difficult-to-control hypertension are few, and strategies
are based largely on observational data from specialty clinics.
These series and clinical experiences suggest that a careful
evaluation of a patient's adherence to
and adequacy of therapy and lifestyle factors often reveals modifiable contributors to refractory
blood pressure; secondary causes (including exogenous substances)
must also be considered. A suboptimal medical regimen has been shown
to be the primary
cause of resistant
hypertension in a majority of patients in these
studies. Figure 1 outlines a suggested approach to
evaluation.


Diagnosis
Blood pressure
should be measured after a patient has been seated quietly for five
minutes, with his or her arm supported at heart level and with the
use of a properly calibrated and sized cuff. If the cuff is too
narrow or too short, readings may be erroneously high (typically by
5 to 15 mm
Hg in the case of systolic pressure). The patient should be asked
whether he or she has smoked a cigarette within the previous 15 to
30 minutes, since smoking can cause an elevation in systolic blood
pressure of 5 to 20 mm
Hg. Avoidance of coffee is also recommended, although the increase
in systolic blood pressure after one cup of caffeinated coffee is
usually only 1 to 2
mm Hg. Long-term smoking or coffee drinking does not
cause persistently elevated blood pressure.
The diagnosis is
based on the findings of at least two or three elevated
blood-pressure measurements (in the physician's office or at home),
despite adherence to regimens containing three medications. However,
if the blood pressure is above 160/100 mm Hg, additional readings
are not necessary for diagnosis. Evaluation (including physical
examination and laboratory testing) is routinely warranted to look
for evidence of end-organ damage related to hypertension (Table 1) and for other cardiovascular risk factors.1 Volume overload and elevated
sympathetic tone, which are common in patients with uncontrolled
blood pressure, may occasionally be suggested by the presence of a
rapid pulse rate. Renin levels have not been found to be useful in
the prediction of excess volume, though they may be useful in the
evaluation of possible secondary causes of hypertension.
 Some patients who have what appears to be resistant hypertension
have a normal blood pressure at home. This phenomenon has been attributed
to transitory, or "white-coat," resistant hypertension
in the physician's office. Repeated home measurements or 24-hour ambulatory
monitoring may differentiate this type of hypertension from
truly resistant hypertension.13 Such measures are warranted in patients undergoing treatment
who have consistently high blood-pressure levels in the physician's
office yet have no evidence of target-organ damage. In one study, as
many as a third of patients with apparently resistant
hypertension had average blood-pressure levels of
less than 130/85 mm Hg on 24-hour or home measurement.14 Some data suggest that blood-pressure values obtained at
home or during 24-hour ambulatory procedures correlate better with
target-organ involvement, especially left ventricular hypertrophy,
than do values obtained in the physician's office.15 However, office, or white-coat, hypertension is not
benign and should not be ignored.
Some patients who have what appears to be resistant hypertension
have a normal blood pressure at home. This phenomenon has been attributed
to transitory, or "white-coat," resistant hypertension
in the physician's office. Repeated home measurements or 24-hour ambulatory
monitoring may differentiate this type of hypertension from
truly resistant hypertension.13 Such measures are warranted in patients undergoing treatment
who have consistently high blood-pressure levels in the physician's
office yet have no evidence of target-organ damage. In one study, as
many as a third of patients with apparently resistant
hypertension had average blood-pressure levels of
less than 130/85 mm Hg on 24-hour or home measurement.14 Some data suggest that blood-pressure values obtained at
home or during 24-hour ambulatory procedures correlate better with
target-organ involvement, especially left ventricular hypertrophy,
than do values obtained in the physician's office.15 However, office, or white-coat, hypertension is not
benign and should not be ignored.
Rarely, in older
patients, what appears to be refractory hypertension may
represent inaccurate measurement owing to severely sclerotic arteries
(i.e., pseudohypertension). The condition is suggested if
the radial pulse remains palpable despite occlusion of the brachial
artery by the cuff (the Osler maneuver),16 although this sign is not specific. The presence of this
condition can be confirmed by intra-arterial blood-pressure
measurement.
Adherence to Treatment
Because a diagnosis
of resistant hypertension requires a finding
of elevated blood pressure despite the use of adequate doses of
at least three medications, the patient's adherence to therapy and
the adequacy of the dose should be evaluated routinely. Studies have
reported that medication was not increased in more than 50 percent
of patients with poorly controlled hypertension
despite repeated office visits. Some patients take less than the
prescribed dose of medication for economic or other reasons. However,
side effects have not been found to be an important reason for a
lack of adherence to therapy but may contribute to nonadherence.
Signs suggesting nonadherence include missed office visits and a
lack of physiological evidence of therapy (e.g., rapid heart rate
despite the prescription of beta-blockers or verapamil), but
nonadherence is often difficult
to recognize or exclude objectively.
Interfering or Exogenous Substances
Patients should be
asked routinely about the use of medications or other substances
that can elevate blood pressure or antagonize the effects of
antihypertensive drugs. These substances include sympathomimetic
drugs (e.g., ephedra, phenylephrine, cocaine, and amphetamines),
herbal supplements (e.g., ginseng and yohimbine), anabolic steroids,
appetite suppressants, and erythropoietin, although all these drugs
probably account for less than 2 percent of cases of resistant hypertension. Nonsteroidal
antiinflammatory drugs and cyclooxygenase-2 inhibitors may raise
both systolic and diastolic blood pressure by several mm Hg. These
agents impair the excretion of sodium, which causes volume retention;
they also inhibit the production of local renal vasodilative prostaglandins;
the therapeutic action of angiotensin-converting–enzyme (ACE)
inhibitors and loop diuretics (but not calcium-channel blockers)
depends on the availability of these prostaglandins.19,20 Efforts should be made to discontinue
such agents, although if they are needed for another condition,
antihypertensive therapy may need to be modified.
An assessment of
dietary and lifestyle factors is also important. Excessive alcohol
use (more than three or four drinks per day) and a high sodium
intake (typically defined by a urinary sodium excretion of more than
150 mmol per day) may contribute to resistant
hypertension;
the frequency of salt sensitivity is increased among patients who
are at least 60 years of age, patients who are black or obese, and
patients with renal impairment. Studies indicate that more than 40
percent of patients with resistant
hypertension
are obese,23,24 and obese patients may require higher doses of
antihypertensive medications than do nonobese patients.
Evaluation of Secondary Hypertension
The possibility that
an underlying condition is causing hypertension
must also be considered; secondary hypertension
is often unmanageable until the underlying cause is treated.11 Among 4000 patients with resistant hypertension
who were evaluated during an 18-year period at one tertiary center,
secondary causes were found in 10 percent of patients overall and in
17 percent of patients over the age of 60 years.25
Chronic renal
parenchymal disease, usually resulting from diabetic nephropathy or
hypertensive nephrosclerosis, may be the most common cause of
secondary hypertension.
Atherosclerotic renovascular disease, which is particularly
prevalent among elderly smokers, is another possible cause. The
presence of an abdominal bruit or hypokalemia or a recent increase
in the severity of hypertension may suggest the
diagnosis of atherosclerotic renovascular disease. Screening for
renovascular disease may be warranted if other causes of resistant hypertension are not identified,
since angioplasty and stenting may improve blood pressure. However,
in cases of renovascular hypertension
caused by atherosclerotic disease, blood pressure often remains
high even after intervention, in contrast to hypertension caused by the much less
common fibromuscular dysplasia.
Table 2 summarizes features of and screening tests for these and
other causes of secondary hypertension,
such as primary aldosteronism (considered to be more common than
previously recognized), pheochromocytoma, and sleep apnea (recently
recognized to be associated with refractory hypertension). Generally,
the decision to screen a patient for such disorders should depend on
suggestive findings on history taking, physical examination, or
basic laboratory testing. Interventions that are directed at these
disorders (e.g., surgery or aldosterone-antagonist therapy for
hyperaldosteronism, surgery for pheochromocytoma, and continuous
positive airway pressure for sleep apnea) may substantially
decrease, although not always normalize, blood pressure. A detailed
discussion of all the causes of secondary hypertension is available elsewhere.

Treatment
Patients should
routinely be encouraged to reduce their intake of sodium, lose
weight (if appropriate), engage in moderate exercise, and reduce
their intake of alcohol (to no more than two to three drinks per
day). The degree of blood-pressure lowering expected with each of
these approaches is often modest but clinically important — for
example, 2 to 8 mm
Hg with dietary sodium restriction (with a goal of urinary sodium
excretion of less than 100 mmol per day), 2 to 4 mm Hg with reduced alcohol
consumption, and 4 to 9
mm Hg with regular physical activity (such as walking
briskly for 30 to 45 minutes daily).
Adherence to therapy
may be increased by the initiation of a system of follow-up
reminders or telephone contacts. The involvement of nurses or nurse
practitioners, who may have more time than a physician to discuss
potential side effects of medications, has been shown to improve
patients' control of their blood pressure. The use of combination
therapy (two medications in one pill) may also improve adherence
and, in some cases, may reduce the cost of care.
Few data from
randomized trials are available to guide the choice of regimen for
patients whose blood pressure remains high even though they take
several medications; recommendations are based largely on
physiological principles and clinical experience. Because volume
overload is common among such patients, the most important
therapeutic maneuver is generally to add or increase diuretic
therapy; more than 60 percent of patients with resistant hypertension may have a response to this approach.
Thiazide diuretics are effective in doses of 12.5 to 25.0 mg daily
if renal function is normal. Experience suggests that a daily dose
of 25 to 50 mg will result in a further decrease in blood pressure.
If the glomerular filtration rate is below 30 to 50 ml per minute
(or the serum creatinine level is more than 1.5 mg per deciliter),
loop diuretics should be used. Short-acting loop diuretics, such as
furosemide (at a dose of 20 to 80 mg daily) or bumetanide (at a dose
of 0.5 to 2.0 mg daily), must be given two or three times per day.
Intermittent natriuresis with once-daily drug administration may
lead to reactive sodium retention mediated by the renin–angiotensin
system, with consequent inadequate blood-pressure control.
Longer-acting diuretics such as torsemide (at 2.5 to 5.0 mg) may be
given once a day but are more expensive.
A generally useful
strategy is to combine agents from various classes, each of which
has one or more of the following effects: a reduction in volume
overload (diuretics and aldosterone antagonists), a reduction in
sympathetic overactivity (beta-blockers), a decrease in vascular
resistance (through the inhibition of the renin–angiotensin system
with the use of ACE inhibitors or angiotensin-receptor blockers),
the promotion of smooth-muscle relaxation (dihydropyridine calcium-channel
blockers and alpha-blockers), and direct vasodilation (hydralazine
and minoxidil), although the latter are less well tolerated. An
additional medication with a different mechanism of action from
others the patient is receiving may further lower the blood pressure
or overcome compensatory changes in blood-pressure elevation caused
by the first medication without increasing adverse effects. For
example, adding a beta-blocker or ACE inhibitor may counteract the
stimulation of the renin–angiotensin system by diuretics.34
Some logical
combinations include a diuretic with an ACE inhibitor, a
beta-blocker, or an angiotensin-receptor blocker or an ACE inhibitor
with a calcium-channel blocker. Most patients with resistant hypertension are already receiving
combinations of these agents. In these instances, it may be
necessary to increase the dose or the frequency of administration
from once to twice daily or to include an additional drug, such as
an aldosterone antagonist if a patient is already receiving a
diuretic, an ACE inhibitor, and a calcium-channel blocker. Certain
medications may be preferred if the patient has coexisting illnesses
(Table 1 of the Supplementary Appendix, which is available with the full text of this article at
www.nejm.org). For example, the addition of an angiotensin-receptor
blocker, a beta-blocker, or an aldosterone antagonist would be
reasonable if the drug is not already being used in a patient with
heart failure.
The Figure below summarizes one approach to the optimization of drug therapy
in patients with resistant
hypertension. There
are limited data to guide whether some agents should be stopped
before others are added if multiple drugs are inadequate.

If resistant hypertension persists, patients can
augment their therapy with an agent from a different class of drugs. For
example, if the patient is receiving an angiotensin-converting–enzyme (ACE)
inhibitor or an angiotensin-receptor blocker (ARB) plus a diuretic and a
beta-blocker, a dihydropyridine calcium-channel blocker can be added. If the
patient is receiving an ACE inhibitor or an ARB plus a diuretic and a
dihydropyridine calcium-channel blocker, a beta-blocker can be added. The
practitioner may consider adding an aldosterone antagonist to any of the
combinations (but with extreme caution if the patient is receiving an ACE
inhibitor or an ARB because of concern regarding hyperkalemia).
Combined alpha- and
beta-blockers (labetalol and carvedilol) may improve blood-pressure
control. Centrally acting agents — for example, clonidine,  2-adrenergic blockers, reserpine (in low doses), and direct
vasodilators (hydralazine or, in rare cases, minoxidil) — may be necessary
in some cases, as tolerated. With direct vasodilators, concomitant
high-dose beta-blockers (metoprolol or atenolol) and loop diuretics
(furosemide) will be needed to counteract reflex tachycardia and
edema. Aside from the aldosterone antagonist spironolactone and
alpha-blockers, which have been shown to reduce blood pressure in
patients with resistant
hypertension, data are
lacking to predict the magnitude of further blood-pressure reduction
associated with the addition of one of these other medications;
clinical experience suggests a decrease in systolic pressure of
about 5 to 10 mm
Hg.
2-adrenergic blockers, reserpine (in low doses), and direct
vasodilators (hydralazine or, in rare cases, minoxidil) — may be necessary
in some cases, as tolerated. With direct vasodilators, concomitant
high-dose beta-blockers (metoprolol or atenolol) and loop diuretics
(furosemide) will be needed to counteract reflex tachycardia and
edema. Aside from the aldosterone antagonist spironolactone and
alpha-blockers, which have been shown to reduce blood pressure in
patients with resistant
hypertension, data are
lacking to predict the magnitude of further blood-pressure reduction
associated with the addition of one of these other medications;
clinical experience suggests a decrease in systolic pressure of
about 5 to 10 mm
Hg.
Referral to a hypertension specialist should be
considered in patients whose hypertension
is difficult to
control despite an assessment of adherence, dose, and other factors
that may exacerbate the condition — particularly if the use of the
above-mentioned combinations is not helpful. In truly refractory cases,
other combinations of medications may be considered. Combinations
that have been studied include dual diuretic therapy (spironolactone
at a dose of 25 to 50 mg daily plus a thiazide at a dose of 12.5 to
50 mg daily or a loop diuretic), which has been associated with a
reduction in systolic blood pressure of 20 to 25 mm Hg and in diastolic
pressure of 10 to 12 mm
Hg (larger decreases than those obtained with the use of a single
diuretic)27; dual calcium-channel blockers (a dihydropyridine, such as
amlodipine, plus a nondihydropyridine), which has been associated
with a reduction in systolic blood pressure of 6 mm Hg and a
reduction in diastolic pressure of 8
mm Hg, as compared with nifedipine alone35; and a combination of an ACE inhibitor and an
angiotensin-receptor blocker, which has been associated with a
reduction in systolic blood pressure of 5 to 6 mm Hg, as
compared with either agent alone.36
However,
the risks of such regimens must be considered (e.g., hyperkalemia
with the ACE inhibitor plus an angiotensin-receptor blocker).
Guidelines
European Society of Hypertension - European Society of
Cardiology Guidelines
7th JNC (American) Guidelines
British Hypertension Society Guidelines IV
Guidelines synthesis
The Seventh
Report of the Joint National Committee on Prevention, Detection,
Evaluation, and Treatment of High Blood Pressure emphasizes the need
to consider secondary causes, improper blood-pressure measurement,
volume overload, competing substances, obesity, nonadherence to
treatment, inadequate doses or inappropriate combinations of
medications, and alcohol consumption as factors in resistant hypertension.1 These
guidelines do not include specific recommendations regarding when or
how to evaluate patients for specific secondary causes of resistant hypertension or for the
management of truly resistant
cases.
Areas of
Uncertainty
Several
questions require further investigation.37 The true
prevalence of resistant
hypertension remains
uncertain. More information is needed to determine the optimal
evaluation of patients for secondary hypertension, including indications for screening
for hyperaldosteronism, which appears to be underdiagnosed. Data
from randomized trials are needed to improve the treatment of
patients whose blood pressure remains high while they are receiving
multiple agents. In such patients, the possible role of new drugs,
such as inhibitors of renin and endothelin-1, requires evaluation.
Summary and
Recommendations
The patient
in the vignette has elevated blood pressure, despite taking three
medications, with evidence of target-organ injury (retinal
arteriopathy and left ventricular hypertrophy). Careful assessment
of her adherence to therapy is warranted. Such adherence may be
improved by addressing the reasons for nonadherence, such as side
effects or the cost of medications, or by arranging for more
frequent office visits or telephone contact. The ibuprofen she takes
for osteoarthritis should probably be discontinued, since it may
contribute to blood-pressure elevation, and be replaced with
acetaminophen. Weight loss and a restriction of dietary sodium
should be encouraged. Since volume overload is common in refractory hypertension, she could increase her
dose of diuretic (with repletion of potassium as needed). If these
interventions are ineffective, a different class of drug (e.g., a
calcium-channel blocker) could be added, and the patient could be
screened for renovascular hypertension,
even though in patients with this condition, blood pressure may
remain elevated despite intervention. Regular follow-up is
warranted, with a goal of maintaining the blood pressure below
140/90 mm Hg.
Hypertensive
Retinopathy
Hypertensive
retinopathy is a condition characterized by a spectrum of retinal
vascular signs in people with elevated blood pressure.1 The detection
of hypertensive retinopathy with the use of an ophthalmoscope
has long been regarded as part of the standard evaluation of
persons with hypertension.2,3,4 This
clinical practice is supported by both previous5 and current6 reports of the Joint
National Committee on Prevention, Detection, Evaluation, and Treatment
of High Blood Pressure (JNC), which list retinopathy as one of
several markers of target-organ damage in hypertension. On the basis
of the JNC criteria, the presence of retinopathy may be an
indication for initiating antihypertensive treatment, even in
people with stage 1 hypertension (blood pressure, 140 to 159/90 to
99 mm Hg) who have no other evidence of target-organ damage.
Despite the JNC
recommendation, the clinical implications of hypertensive retinopathy are unclear. Many
physicians do not regularly perform an ophthalmoscopic examination
as part of the care they provide to hypertensive patients, nor do they include
retinal findings when making decisions about treatment. Furthermore,
there is no clear consensus regarding the classification of hypertensive retinopathy or whether a retinal
examination is useful for risk stratification.
The evidence
in support of the JNC guidelines on retinal findings in hypertension
is based on earlier studies that may not have direct relevance to
current clinical practice.7,8,9,10 These studies
have several important limitations. First, because they involved
patients who had uncontrolled and untreated hypertension, generalization
to contemporary populations of patients with lower blood-pressure
levels may be problematic. Second, retinopathy
as defined in these studies was based on a direct ophthalmoscopic examination.
This technique has been shown to be unreliable, with high rates of
interobserver variability (20 to 42 percent) and intraobserver
variability (10 to 33 percent) when used in persons with mild
hypertension.11,12 Third,
although many earlier studies cite increased mortality among persons
with hypertensive
retinopathy,8,9,10 few studies
have demonstrated associations between hypertensive retinopathy and specific
cardiovascular outcomes (e.g., incident stroke and coronary heart
disease) or have adequately controlled for relevant confounding
factors (e.g., hyperlipidemia and cigarette smoking). Thus, whether
hypertensive retinopathy predicts the risk of
cardiovascular outcomes independently of other risk indicators has
not been examined until recently. The purpose of this review is to
appraise recent studies (i.e., from 1990 onward) in regard to the
pathophysiology, epidemiology, and cardiovascular associations of hypertensive retinopathy and the evidence that
supports its use for risk stratification in persons with
hypertension.
Historical
Context and Classification
Hypertensive
retinopathy was first described by Marcus Gunn in the 19th
century in a series of patients with hypertension and renal
disease.7 The retinal
signs he observed included generalized and focal arteriolar
narrowing, arteriovenous nicking, flame-shaped and
blot-shaped retinal hemorrhages, cotton-wool spots, and swelling of
the optic disk (Figure 1, Figure 2, and Figure 3). In 1939,
Keith et al. showed that these signs of retinopathy were
predictive of death in patients with hypertension.10 The authors
described a widely used classification system that categorized these signs
into four groups of increasing severity.
Examples of Mild Hypertensive Retinopathy.Panel A shows arteriovenous nicking
(black arrow) and focal narrowing (white arrow). Panel B shows arteriovenous nicking
(black arrows) and widening or accentuation ("copper wiring") of the
central light reflex of the arterioles (white arrows).

Examples
of Moderate Hypertensive Retinopathy. Panel A shows
retinal hemorrhages (black arrows) and a cotton-wool spot (white arrow). Panel
B shows cotton-wool spots (white arrows) and arteriovenous nicking (black
arrows).

Example of Malignant Hypertensive Retinopathy. Multiple
cotton-wool spots (white arrows), retinal hemorrhages (black arrows), and
swelling of the optic disk are visible.

However,
several reviews of hypertensive
retinopathy since 1996
have questioned the usefulness of the classification system by
Keith et al. (subsequently modified by Scheie) and its relevance to
current clinical practice. The major criticisms of the original and
modified classifications are that they do not enable the clinician
to distinguish among low retinopathy
grades (e.g., grade 1 signs are not easily distinguished from grade
2 signs) and that the retinopathy
grades are not closely correlated with the severity of hypertension.
Furthermore, a detailed categorization of retinopathy into four grades does
not appear to be supported by retinal studies with the use of
fluorescein angiography.
Pathophysiology
The retinal
circulation undergoes a series of pathophysiological changes in
response to elevated blood pressure. In the initial, vasoconstrictive
stage, there is vasospasm and an increase in retinal arteriolar tone
owing to local autoregulatory mechanisms. This stage is seen
clinically as a generalized narrowing of the retinal arterioles.
Persistently elevated blood pressure leads to intimal thickening,
hyperplasia of the media wall, and hyaline degeneration in the
subsequent, sclerotic, stage. This stage corresponds to more severe
generalized and focal areas of arteriolar narrowing, changes in the
arteriolar and venular junctions (i.e., arteriovenous nicking or
nipping), and alterations in the arteriolar light reflex (i.e.,
widening and accentuation of the central light reflex, or
"copper wiring").
This is
followed by an exudative stage, in which there is disruption of the
blood–retina barrier, necrosis of the smooth muscles and endothelial
cells, exudation of blood and lipids, and retinal ischemia. These
changes are manifested in the retina as microaneurysms, hemorrhages,
hard exudates, and cotton-wool spots. Swelling of the optic disk may
occur at this time and usually indicates severely elevated blood
pressure (i.e., malignant hypertension). Because better methods for
the control of blood pressure are now available in the general
population, malignant hypertension is rarely seen. In contrast,
other retinal vascular complications of hypertension, such as
macroaneurysms and branch-vein occlusions, are not uncommon in
patients with chronically elevated blood pressure. The stages of hypertensive retinopathy described here, however,
may not be sequential. For example, signs of retinopathy that reflect
the exudative stage, such as retinal hemorrhage or microaneurysm,
may be seen in eyes that do not have features of the sclerotic stage
(e.g., arteriovenous nicking). The exudative signs are nonspecific,
since they are seen in diabetes and other conditions.
Epidemiology
Since 1990,
there have been seven population-based epidemiologic studies
(involving a total of 26,477 participants) of various signs of hypertensive retinopathy. In all seven
studies, retinal photographs were used to define specific signs of retinopathy without regard to a
predetermined grading system. All of the studies were conducted in
the general community and included persons with and those without a
history of hypertension.
In general,
these studies show that signs of hypertensive
retinopathy can
be reliably identified with a standardized examination of photographs
of the fundus. Reproducibility was substantial for the grading of
retinal hemorrhages and microaneurysms (e.g.,  =0.80 to 0.99) and fair to moderate for the grading of
arteriovenous nicking and focal arteriolar narrowing (
=0.80 to 0.99) and fair to moderate for the grading of
arteriovenous nicking and focal arteriolar narrowing ( =0.40 to 0.79). In four populations,
generalized arteriolar narrowing was estimated from an assessment of
retinal vessel diameters with the use of digitized photographs. This
technique appears to have substantial reproducibility (i.e., the
intraclass correlation coefficient ranged from 0.80 to 0.99 in four
studies).
=0.40 to 0.79). In four populations,
generalized arteriolar narrowing was estimated from an assessment of
retinal vessel diameters with the use of digitized photographs. This
technique appears to have substantial reproducibility (i.e., the
intraclass correlation coefficient ranged from 0.80 to 0.99 in four
studies).
On the basis
of photographic grading, these epidemiologic studies show that signs
of hypertensive retinopathy are common in people
40 years of age or older, even in those without a history of hypertension.
Prevalence rates ranged from 2 to 15 percent for various signs of retinopathy, in contrast to the
earlier report from the Framingham Eye Study that found a prevalence
of less than 1 percent among participants who underwent an
ophthalmoscopic examination with dilation. The higher rates of
prevalence in these more recent studies are probably due to a higher
sensitivity of photography, as compared with clinical ophthalmoscopy,
for detecting certain signs of retinopathy.
However, there have been no studies that have directly compared the
sensitivity or reliability of photography with that of ophthalmoscopy for
the detection of hypertensive
retinopathy, as there
have been for diabetic retinopathy.
A higher
prevalence of retinopathy
has been reported among black persons than among whites, a
difference that is explained in large part by the higher levels of
blood pressure among blacks. The racial variation confirms the
results of a previous population-based survey that used direct
ophthalmoscopy34 and suggests
that retinal examination may be particularly useful for risk
stratification among blacks. Variations in the prevalence of
specific signs of hypertensive
retinopathy according
to age and sex have not been consistently demonstrated. There have
been fewer studies of the incidence of hypertensive retinopathy.
Two studies indicate that the incidence of various signs of retinopathy over a period of five to
seven years ranges from 6 to 10 percent.
Blood
Pressure
Numerous
studies have confirmed the strong association between the presence
of signs of hypertensive
retinopathy and
elevated blood pressure. Two studies have further evaluated
the effect of a history of elevated blood pressure on the occurrence
of specific retinal signs. In both studies, generalized retinal
arteriolar narrowing and arteriovenous nicking were associated with
an elevation in blood pressure that had been documented six to eight
years before the retinal assessment; the studies were controlled for
concurrent blood-pressure levels. This association suggests that
generalized narrowing and arteriovenous nicking are markers of
vascular damage from chronic hypertension. In contrast, other signs
(focal arteriolar narrowing, retinal hemorrhages, microaneurysms,
and cotton-wool spots) were related to current but not previous
blood-pressure levels and may therefore be more indicative of the
severity of recent hypertension.
Furthermore,
the observation of signs of retinopathy
in people without a known history of hypertension suggests that
these signs may be markers of a prehypertensive state. For example, generalized
and focal narrowing of the retinal arterioles has been shown to
predict the risk of hypertension in normotensive persons.38 Other factors
unrelated to hypertension (e.g., hyperglycemia, inflammation, and
endothelial dysfunction24) may also be
involved in the pathogenesis of retinopathy.
The Risk of
Stroke
The strongest
evidence of the usefulness of an evaluation of hypertensive retinopathy for risk stratification
is based on its association with stroke. It is well known that the
retinal circulation shares anatomical, physiological, and
embryologic features with the cerebral circulation. An autopsy study
of patients with stroke showed a close correlation between retinal
and cerebral arteriolar findings. Functional alterations in retinal
blood flow in patients with lacunar stroke have also been reported.40
Epidemiologic
data from four large, population-based studies showed independent
associations between signs of hypertensive
retinopathy, as
defined by the findings on retinal photographs, and the risk of
stroke. The Atherosclerosis Risk in Communities study, a multisite
cohort study, showed that some signs of retinopathy
(e.g., retinal hemorrhages, microaneurysms, and cotton-wool spots)
were associated with a risk of newly diagnosed clinical stroke that
was two to four times as high as that for patients who did not have
these signs, even when the analysis was controlled for the effects
of long-term elevations in blood pressure, cigarette smoking,
elevated lipid levels, and other risk factors for stroke. This study
has also shown that signs of retinopathy
are associated with reduced cognitive performance on standardized
neuropsychological tests, cerebral white-matter lesions, and
cerebral atrophy as defined on the basis of findings on magnetic
resonance imaging (MRI).
In the
Atherosclerosis Risk in Communities study, the five-year relative
risk of stroke among participants who had both hypertensive retinopathy and cerebral lesions on MRI, as compared
with those who had neither of these findings, was 18.1 (95 percent
confidence interval, 5.9 to 55.4); among participants who had
white-matter lesions only, the relative risk of stroke was 3.4 (95
percent confidence interval, 1.5 to 7.7). This pattern appears to
reflect more severe or extensive subclinical cerebral microvascular disease
in persons with both cerebral and retinal markers of hypertensive end-organ damage. In
the Cardiovascular Health Study, after the analysis was controlled
for elevated blood pressure and risk factors, persons with similar
signs of retinopathy
(retinal hemorrhages, microaneurysms, and cotton-wool spots) were
twice as likely to have a history of stroke as were those who did
not have these signs (odds ratio, 2.0; 95 percent confidence interval,
1.1 to 3.6). Population-based studies in Wisconsin and in Japanhave
shown that the risks of fatal and nonfatal stroke are two to three
times as high in persons with signs of retinopathy as they are in persons
who do not have these signs — an association that is independent of
cardiovascular risk factors.
These
population-based studies also show substantially weaker and less
consistent associations between other retinal changes (e.g.,
generalized and focal narrowing of the arterioles and arteriovenous
nicking) and stroke, death from stroke, cognitive impairment, and
cerebral changes on MRI. The retinal
signs most strongly associated with stroke (i.e., retinal hemorrhages,
microaneurysms, and cotton-wool spots) are correlated
with a breakdown of the blood–retina barrier. The association
of these signs with stroke may therefore suggest that disruption of
the blood–brain barrier is a possible pathophysiological feature in
the development of cerebrovascular disease. These findings also
support the concept that an assessment of specific signs, rather
than the presence or absence of hypertensive
retinopathy, may
be important for risk stratification.
The Risk of Coronary
Heart Disease
There are
fewer data regarding the association of hypertensive
retinopathy and
the risk of coronary heart disease. In the National Health
Examination Survey, persons with retinal arteriolar narrowing, as
detected on ophthalmoscopy, were two to six times as likely to have
preexisting coronary heart disease as those without these changes,
after the analysis was controlled for the presence or absence of
hypertension and diabetes and for serum cholesterol levels. In a
study of 560 men with hypertension and hyperlipidemia, the presence
of hypertensive retinopathy predicted a doubling
of the risk of coronary heart disease (relative risk, 2.1; 95 percent
confidence interval, 1.0 to 4.2), and the presence of either
generalized or focal narrowing of the arterioles predicted almost a
tripling of this risk (relative risk, 2.9; 95 percent confidence
interval, 1.3 to 6.2). In contrast, the Atherosclerosis Risk in
Communities study showed that generalized narrowing of the retinal
arterioles was associated with subsequent coronary heart disease in
women (relative risk, 2.2; 95 percent confidence interval, 1.0 to
4.6) but not in men (relative risk, 1.1; 95 percent confidence
interval, 0.7 to 1.8). This finding may reflect the higher risk of
coronary microvascular disease among women than among men.
Treatment
Some
experimental studies and clinical trials have shown that signs of hypertensive retinopathy regress with the control
of blood pressure, although spontaneous resolution of these signs in
the presence of high blood pressure has also been reported.54 It is
unclear whether antihypertensive
medications that are thought to have direct beneficial effects on
the microvascular structure (e.g., angiotension-converting–enzyme
inhibitors) would reduce the damage of retinopathy beyond the reduction
effected by lowered blood pressure. In a small study of 28 patients with
mild hypertension who were randomly assigned to receive treatment
with enalapril or hydrochlorothiazide, opacification of the retinal
arteriolar wall was significantly reduced after 26 weeks of
treatment with enalapril; no other signs of retinopathy were reduced.53 In contrast,
hydrochlorothiazide did not have any effect on the signs of retinopathy. However, to date, there
are no data from prospective, controlled trials that demonstrate that
the specific reduction of hypertensive
retinopathy also reduces
the morbidity and mortality associated with cardiovascular disease.
It is also unclear whether the targeting of persons with hypertensive retinopathy for established
risk-reducing interventions offers additional advantages over the
use of strategies without regard to retinal findings.
Future
Research
The recent
data suggest that there are several lines of future research. First,
a standardized classification system for hypertensive
retinopathy
should be developed that is relevant to contemporary clinical
situations and reflects the recent data. Evidence from recent
studies supports the development of a photographic classification system
that would be similar to the photographic grading of diabetic retinopathy. However, it is not yet
clear that retinal photography should be a routine part of the
management of hypertension or that photography is superior to
ophthalmoscopy for the detection of signs of hypertensive retinopathy.
Second,
additional prospective studies are needed that demonstrate independent
associations of hypertensive
retinopathy with
various cardiovascular outcomes. For example, there are no recent
studies focusing on whether signs of retinopathy predict other hypertensive complications,
such as renal dysfunction or congestive heart failure. It is also
unclear whether a retinal examination would confer a greater benefit
in specific subgroups of populations (e.g., younger people,45 women,49 and blacks33). An ongoing
longitudinal study involving a multiethnic population will provide further
insights into these issues.54
Third, it is
important to compare the relative value of a retinal assessment
(based on an ophthalmoscopic examination performed with or without
the use of photography) with other strategies of risk stratification
(e.g., the use of electrocardiography and echocardiography).
Finally, there is a need to evaluate whether specific therapy that
is focused on the retinal microcirculation can reverse changes in retinopathy, and, if so, whether
this approach will also ultimately result in a reduced
cardiovascular risk.
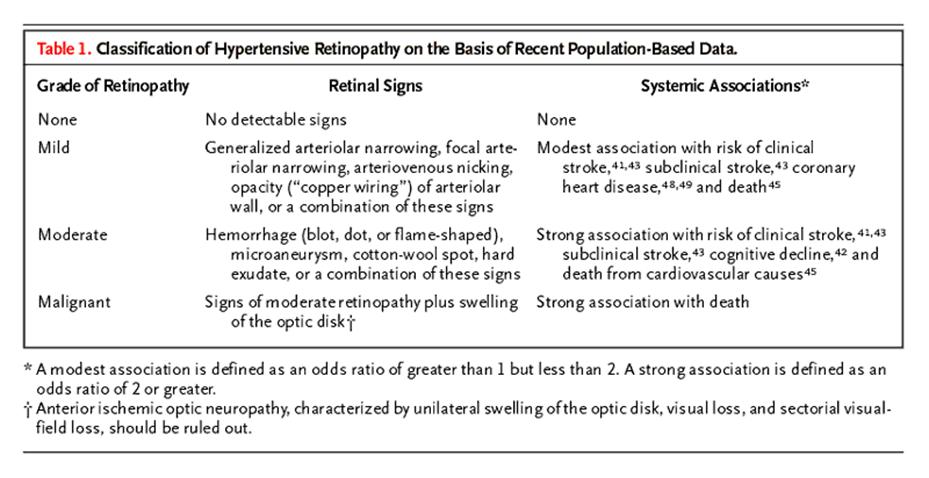
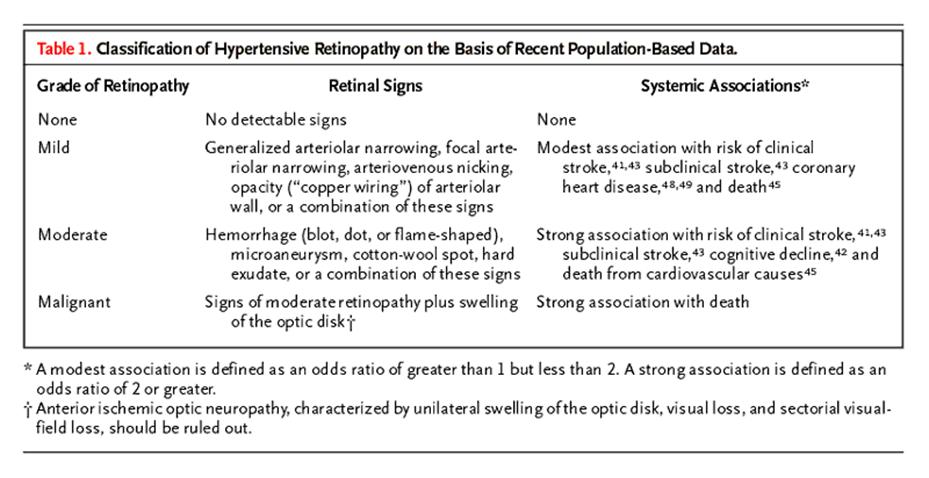
The Clinical
Approach
How should
the physician use the available evidence? This review provides
compelling evidence that certain signs of hypertensive retinopathy are associated with an increased
cardiovascular risk that is independent of other risk factors. On
the basis of the strength of these reported associations, we propose
a simplified classification of hypertensive retinopathy
— none, mild, moderate, and malignant — according to the severity
of the retinal signs (Table 1). The
physician may continue to provide routine care for patients with no retinopathy, undertake more
vigilant monitoring of the cardiovascular risk in patients with mild
retinopathy (i.e.,
those who have retinal arteriolar signs only), or adopt an
aggressive approach to risk reduction in patients with moderate retinopathy (Figure 4). The few
patients who have swelling of both optic disks and very high blood
pressure (i.e., malignant retinopathy)
need urgent antihypertensive
treatment. In hypertensive patients with swelling
of the optic disk, the physician should rule out anterior ischemic
optic neuropathy, which occurs more frequently than malignant hypertensive retinopathy and is
typically manifested as unilateral disk swelling, visual loss, and
defects of the sectorial visual fields.

There is
insufficient evidence to recommend a routine ophthalmoscopic consultation
for all patients with hypertension. If the initial clinical findings
are equivocal (e.g., there is borderline or inconsistent
hypertension with no other evidence of target-organ damage), an
ophthalmoscopic consultation may be useful to supplement the risk
assessment and treatment decisions. For some patients (e.g., those
with diabetes or visual symptoms), referral may also be important to
rule out other conditions such as diabetic retinopathy or retinal-vein
occlusion.
Conclusions
Signs of hypertensive retinopathy are common and are
correlated with elevated blood pressure. Recent studies show that
some of these signs (e.g., retinal hemorrhages, microaneurysms, and
cotton-wool spots) predict stroke and death from stroke independently
of elevated blood pressure and other risk factors. Patients with
these signs of retinopathy
may benefit from close monitoring of cerebrovascular risk and
intensive measures to reduce that risk.
Hypertensive
crises: urgencies and emergencies
Definitions
and probable causes of hypertensive crisis
Hypertensive urgencies
can be defined as severe elevations in BP that do not exhibit evidence of
target-organ (cardiovascular, renal, CNS) dysfunction or damage. Urgencies can
be managed by the administration of oral medications, most often in the
emergency department (ED), and follow-up on an outpatient basis. Hypertensive emergencies
are severe elevations in systolic and diastolic BP associated with acute
target-organ damage that require immediate management in a hospital setting.
Hypertensive
crises encompass a spectrum of clinical situations that have in common blood
pressure (BP) that is elevated, and progressive or
impending target organ damage. Most hypertensive urgencies or emergencies are
preventable and are the result of inadequate treatment of mild-to-moderate
hypertension or nonadherence to antihypertensive therapy.
Some of examples of hypertensive crises
Traditionally,
hypertensive crises have been divided into emergencies and urgencies.
Hypertensive emergencies are severe elevations in blood pressure (BP) that are
complicated by evidence of progressive target organ dysfunction, and will
require immediate BP reduction (not necessarily to normal ranges) to prevent or
limit target organ damage. Examples include: hypertensive encephalopathy,
intracranial hemorrhage, unstable angina pectoris, or
acute myocardial infarction, acute left ventricular failure with pulmonary
edema, dissecting aneurysm, or eclampsia. While the level of BP at the time of
presentation is usually very high (greater than 180/120 mm Hg), keep in mind that
it is not the degree of BP elevation, but rather the clinical status of the
patient that defines a hypertensive emergency. For example, a BP of 160/100 mm
Hg in a 60-year-old patient who presents with acute pulmonary edema represents
a true hypertensive emergency.
Hypertensive
urgencies are severe elevations of BP but without evidence of progressive
target organ dysfunction and would be better defined as severe elevations in BP
without acute, progressive target organ damage. A traditional
term “urgency” has led to aggressive and often excessive treatment of the
majority of patients who present to Emergency Departments (ED) with severe
hypertension. While these patients may present with levels of BP similar to the
hypertensive emergency, and may have evidence of target organ involvement, they
do not display evidence of ongoing progressive target organ damage. Most of
these patients are, in fact, nonadherent to drug therapy or are inadequately
treated hypertensive patients and often present to the ED for other reasons.
Patients with severe elevations of BP can be managed in the ED with oral agents
and appropriate follow-up within 24 hours to several days depending upon the
individual characteristics of the patient. It is the correct differentiation of
these two forms of hypertensive crises, however, that presents the greatest
challenge to the physician.
Initial
Assessment
A brief but thorough history should address the
duration as well as the severity of hypertension, all current medications
including prescription and nonprescription drugs and, of particular importance,
the use of recreational drugs. A history of other comorbid conditions and prior
cardiovascular or renal disease is essential to the initial evaluation. Direct
questioning regarding the level of compliance with current antihypertensive
medications may establish inadequacy of treatment or frank noncompliance.
Frequent or
continuous monitoring of BP should be established. Look for historical
information suggestive of neurologic,
cardiovascular, and/or renal symptoms. Check for specific manifestations such
as headache, seizures, chest pain, dyspnea, and edema. The clinical
characteristics of a hypertensive emergency are listed here. The level of BP alone does not
determine a hypertensive emergency; rather, it is the degree of target organ
involvement that will determine the rapidity with which BP should be reduced to
a safer level to prevent or limit target organ damage. Initial therapy will be
for a presumptive diagnosis based on the information available during the
initial triage evaluation.
The attached
algorithm (See algorithm) can help the
clinician identify those patients who meet the criteria of a hypertensive
emergency that requires immediate admission to an ICU for continuous monitoring
of BP and initiation of parenteral antihypertensive therapy. For patients with
uncontrolled hypertension (urgency), evidence of target organ damage may or may
not be present but these patients do not demonstrate any evidence of
deterioration of target organ function. They can be observed for several hours
in the ED during which time their oral medications can be resumed, if
discontinued, or if untreated, an oral regimen can be initiated. On occasion,
increasing presently inadequate dosages of medication may be appropriate.
Appropriate outpatient follow-up can then be arranged within 24 hours to
several days as needed, and if no prior evaluation has been performed on this
patient for hypertension, an outpatient appointment should be established.
Failure to follow-up on this large group of patients is a missed opportunity
from the standpoint both of keeping patients in the healthcare system, and
establishing optimal BP.
Physical
Examination
The physical examination should begin with an assessment of BP, with an
appropriate-size cuff in both upper extremities and in a lower extremity if
peripheral pulses are markedly reduced. Brachial, femoral, and carotid pulses
should be assessed. A careful cardiovascular examination as well as a thorough
neurologic examination, including mental status, should be conducted. This
assessment will aid in establishing the degree of involvement of affected
target organs and should provide clues to the possible existence of a secondary
form of hypertension, such as renovascular hypertension. If a secondary cause
of hypertension is suspected, appropriate blood and urine samples should be
obtained before aggressive therapy is initiated. A careful funduscopic examination
should be performed to detect the presence of hemorrhages, exudates, and/or
papilledema.
Initial
Laboratory Studies
Initial laboratory studies should be limited and rapidly expedited. A
urinalysis with microscopic examination of the urinary sediment, an immediate
chemistry panel, and an electrocardiogram should be obtained. The urinalysis
may reveal significant proteinuria, red blood cells, and/or cellular casts.
Cellular casts are suggestive of renal parenchyma disease. Electrolyte
abnormalities, particularly hypokalemia or hypomagnesemia, increase the risk of
cardiac arrhythmias, and the chemistry panel will also provide evidence of
renal and/or hepatic dysfunction. The electrocardiogram should identify
evidence of coronary ischemia and/or left ventricular hypertrophy and may
reveal pulse deficits, raising the question of aortic dissection. When the
clinical examination suggests cerebrovascular ischemia or hemorrhage, or if the
patient is comatose, a computed tomographic scan of the head should be
immediately obtained.
Initial Treatment
of the Hypertensive Emergency
The initial goal for BP reduction is not to obtain a normal BP but rather to
achieve a progressive, controlled reduction in BP to minimize the risk of
hypoperfusion in cerebral, coronary, and renovascular beds. Under normal
conditions, blood flow to these organs remains relatively constant despite wide
fluctuations in BP. In the presence of severe hypertension, the autoregulatory
range is shifted upward so that higher levels of BP are tolerated, but organ
circulation may be put at risk with sudden reductions in BP. As an example,
studies on the autoregulation of cerebral blood flow suggest that the lower
limit of autoregulation is about 25% below the resting mean arterial pressure
in normotensive subjects and in those with uncomplicated essential
hypertension. These observations have led to the suggestion that initial
reduction in mean arterial pressure should not exceed 20% to 25% below the
pretreatment BP. As an alternative, mean arterial pressure can be reduced
within the first 30 to 60 minutes to 110 to 115 mm Hg. If this level of BP is
well tolerated and the patient is clinically stable, further gradual reductions
toward a normal BP can be implemented over the next 24 hours. Excessively rapid
reductions in BP have been associated with acute deterioration in renal
function, ischemic cardiac or cerebral events, and occasional retinal arterial
occlusion and acute blindness.
A significant
exception to the above recommendations should be recognized for patients with
ischemic stroke, with the awareness that cerebral autoregulation is disrupted
in ischemic tissue. There is no clear evidence from clinical trials to support
the use of antihypertensive treatment during an acute stroke in the absence of
other concurrent disorders such as aortic dissection or heart failure.
Antihypertensive treatment may adversely affect cerebral autoregulation in
acute stroke. Hypertension associated with an acute ischemic stroke
spontaneously decreases to pre-stroke levels within several days.
How Urgent is Urgent Hypertension?
Historically, most patients seen in the ED with severe hypertension did not
meet the criteria for hypertensive emergency and were therefore classified as
having hypertensive urgencies. Most were treated aggressively in the ED and
many were, in fact, admitted to the hospital for control of BP. The important
caveat is that elevated blood pressure alone rarely requires emergency therapy.
Initial triage should identify those patients who have an elevated BP without
any evidence of significant target organ damage or any other impending
cardiovascular events, and these patients clearly represent the majority of
those seen in the ED. They are often asymptomatic and can be observed for a
brief period in the ED to initiate or resume medication in the noncompliant patient
or to increase dosages for those being inadequately treated. Follow-up can be
arranged within several days in the outpatient department.
The occasional
patient who presents to the ED with uncontrolled hypertension and symptoms such
as headache, shortness of breath, or epistaxis, may benefit from observation in
the ED over a period of several hours and/or an increase in current medications
or added medication to further lower BP under observation and monitoring of
current symptoms. When clinically stable, the patient may safely be sent home
with oral agents and arrangements for follow-up. There are several oral agents
available that can provide rapid response in blood pressure within one to
several hours. These include agents such as the short-acting ACE inhibitor,
captopril, clonidine, Labetalol, or in selected patients the alpha-adrenergic
blocking agent prazosin. Some of the pharmacologic characteristics of these
oral agents are listed below.
In either case, to
discharge the patient from an ED without a confirmed follow-up appointment
represents a missed opportunity to get that patient back into treatment for
optimal control of BP, which should be a management goal.
There is little justification today to admit patients with hypertensive urgency
or high BP to a hospital for further evaluation and management when these
issues can be efficiently and cost-effectively addressed in the outpatient
setting.
Oral Agents
for Severe Hypertensive
Several oral agents can be particularly appropriate
for treating a hypertensive urgency in the ED.
Captopril,
an angiotensin-converting enzyme inhibitor, is well tolerated and can
effectively reduce BP in a hypertensive urgency. Given
by mouth, captopril is usually effective within 15 to 30 minutes and may be
repeated in 1 to 2 hours, depending on the response. The drug has been
administered sublingually, in which case the onset of action is within 10 to 20
minutes, with a maximal effect reached within 1 hour. Responsiveness to
captopril can be enhanced by the coadministration of a loop diuretic such as
furosemide. Administration may lead to acute renal failure in patients with
high-grade bilateral renal artery stenosis, and some reflex tachycardia may be
observed.
Clonidine
is a centrally acting alpha-adrenergic agonist with onset of action 30 to 60
minutes after oral administration, and maximal effects are usually seen within
2 to 4 hours. This agent is most commonly administered as a loading dose of 0.1
or 0.2 mg followed by 0.1 mg hourly for several hours until an appropriate BP
level is attained. Evidence suggests that a comparable response may be seen
with a single 0.2 mg dose.5
The most common adverse effect in the acute setting is drowsiness, affecting up
to 45% of patients. Clonidine may be a poor choice when monitoring of mental
status is important. Dry mouth is a common complaint, and light-headedness is
occasionally observed.
Labetalol,
a combined alpha- and beta-adrenergic blocking agent, can be effectively
administered orally in a dose of 200 to 400 mg with BP response observed within
2 to 3 hours. However, the onset of effect may be observed within 1 to 2 hours.
Like other beta-blocking agents, labetalol has the potential to induce heart
block and to worsen the symptoms of bronchospasm in the asthmatic patient.
Caution must be observed in patients who have more than first-degree heart
block, symptomatic bradycardia, or congestive heart failure.
Prazosin
is an alpha-adrenergic blocking agent that can have limited benefit in the
early management of a patient with a pheochromocytoma. Side effects include
first-dose syncope, palpitations, tachycardia, and orthostatic hypotension.
Parenteral
Agents for Hypertensive Emergencies
See also Parenteral drugs for hypertensive emergencies
Parental therapy may be initiated in the ED if suitable supervision and monitoring of BP can be provided. More
appropriately, the patient should be admitted to an ICU where monitoring of BP
is available. A number of parenteral agents are effective in treating
hypertensive emergencies (Table).
Labetalol
is effective when administered as 20- to 40-mg bolus intravenous (IV)
injections and can provide a step-wise, controlled reduction in BP to a
predetermined goal. Once the goal BP is achieved, injections are stopped, and
the long duration of action facilitates conversion to effective oral therapy. A
continuous infusion of labetalol at 2 mg/min offers an alternative method of
administration and is also associated with a gradual yet controlled reduction
in BP. Since the beta-blocking effects predominate with this agent, bradycardia
or heart block may be observed in patients with intrinsic heart disease.
Sodium
nitroprusside has an extremely rapid onset of action, within
seconds of initiating an infusion, and a rapid offset of effect within 1 to 2
minutes, which necessitates constant supervision of BP during administration.
This agent is particularly effective in reducing preload and afterload in
patients with impaired left ventricular function, and a carefully titrated
infusion can achieve any desired goal BP. Nitroprusside does not cause sedation
or somnolence but is rapidly degraded by light, requiring periodic exchange of
solutions.
In patients with
significant renal impairment, accumulation of a major metabolite, thiocyanate,
may occur over several days with toxic effects. In the presence of poor tissue
perfusion and depressed hepatic function, an intermediate metabolite in the
form of cyanide can accumulate and occasionally lead to cyanide poisoning.
Nicardipine
is an IV form of the dihydropyridine calcium antagonist and is effective in a
high percentage of hypertensive emergencies, particularly at higher infusion
rates. Its growing popularity can be attributed to its ease of administration.
Infusion rates can be increased by 2.5 mg/hr at intervals of 15 to 20 minutes
until the maximal recommended dosage of 15 mg/hr is obtained or until the desired
reduction in BP is achieved. Dosing of nicardipine is not dependent on body
weight. Nicardipine has been shown to reduce both cerebral and coronary
ischemia although headache, nausea, and vomiting may occasionally be observed.
Nitroglycerin
may be of particular benefit in hypertensive emergencies with coexisting
coronary ischemia. Since this agent dilates collateral coronary vessels and,
like nitroprusside, has a rapid onset and offset of effect, its use requires
close nursing supervision. Unfortunately, at low infusion rates, nitroglycerin
has its primary effect on capacitance vessels in which much higher infusion
rates are required to effect arteriolar
vasodilitation. Infusion rates may be increased at 3- to 5-minute intervals
until the desired effect is achieved. Nitroglycerin may be particularly useful
in patients with severe coronary ischemia whose BPs are only modestly elevated
or in patients with acute hypertension following postcoronary artery bypass
surgery. Tolerance to IV nitroglycerin may be observed within 24 to 48 hours of
instituting an infusion.
Fenoldapam
is a selective, peripheral dopamine1-receptor agonist that induces
systemic vasodilation, particularly in the renal circulation.10
This agent also has effects on renal proximal and distal tubules. Fenoldapam
does not bind to dopamine2 receptors or beta-adrenergic receptors;
it has no alpha-adrenergic agonist effects but is an alpha1
antagonist. This drug does not cross the blood/brain barrier.
Fenoldapam's unique
effects on the kidney provide increased urine flow rate, sodium and potassium
excretion, and improved creatinine clearance, making this agent particularly
attractive in hypertensive emergencies associated with significant renal
impairment.
Fenoldapam
provides clinical effects similar to those of nitroprusside in improving
cardiac hemodynamics in patients with acute congestive heart failure. Onset of
clinical effect is seen within 5 minutes, and effects tend to dissipate within
30 minutes of discontinuing the infusion. The most common side effects include
headache, flushing, tachycardia, and dizziness. A dose-related increase in
intraocular pressure has been observed in normotensive and hypertensive
patients. Inactive metabolites are eliminated in the urine, and no dosage
adjustments are required for patients with renal or hepatic impairment.
Hydralazine
finds limited use today in pregnant women with preeclampsia. Five to 20 mg may
be administered IV as a bolus injection, and may be repeated. The major
advantage is this agent's ability to improve uterine blood flow. Hydralazine is
contraindicated in patients who have coronary atherosclerosis, as
administration is associated with reflex tachycardia and sodium and water
retention, together with intense flushing. Headache and increased intracranial
pressure have also been observed.
Other
Parenteral Agents
Enalaprilat is administered in an IV dose
of 1.25 mg and may be repeated at 6-hour intervals. Onset of action is within
30 minutes. Response to enalaprilat in hypertensive emergencies is
unpredictable, in part because of variable degrees of plasma volume expansion.
This agent may be particularly suitable in hypertensive emergencies associated
with congestive heart failure or with high plasma angiotensin II
concentrations.
Esmolol
is an ultra-short-acting beta-adrenergic blocker that is administered
intravenously. Onset of effect is seen within 1 to 5 minutes, with a rapid
offset of effect within 15 to 30 minutes after discontinuation. Esmolol may be
administered as a 500-µg/kg bolus injection, which may be repeated after 5
minutes. Alternatively, an infusion of 50 to 100 µg/kg/min
may be initiated and increased to 300 µg/kg/min as needed. Adverse effects
include increased heart block, precipitation of congestive heart failure, and
bronchial spasm.
Phentolamine
is a nonselective alpha-adrenergic blocking agent that is still used when
excess catecholamine states, such as pheochromocytoma, are suspected. It is
useful as a diagnostic agent when administered as a bolus injection of 5 to 10
mg in patients with suspected pheochromocytoma. Acute BP lowering will be seen
within several minutes and may last 10 to 30 minutes. Tachycardia is common and
on occasion may precipitate myocardial ischemia. Nitroprusside and labetalol
are more easily titrated in the management of hypertensive emergencies
associated with high circulating levels of catecholamines, and therefore phentolamine
is rarely used therapeutically today.
Diazoxide
is rarely used any longer in the treatment of hypertensive emergencies.
Although a potent vasodilator, large doses of 300 mg were often associated with
severe hypotension. Smaller miniboluses of 50 mg administered at 10- to
15-minute intervals can provide controlled reduction of BP but are usually
associated with reflex tachycardia, hyperglycemia, hyperuricemia, and sodium
and water retention. In view of these side effects, diazoxide offers little
advantage over several other agents that have more acceptable adverse-effect
profiles.
Hypertensive
emergencies can carry a poor prognosis unless the BP is reduced quickly,
whereas hypertensive urgencies pose less immediate danger. Hypertensive
emergencies are considered to be clinical circumstances in which the BP should
be reduced immediately (within a matter of a few hours), whereas in
hypertensive urgencies, BP reduction can be accomplished gradually (within
several hours or even days). There is no arbitrary level of BP that separates
hypertensive emergencies from urgencies. The presence of acute target-organ
damage is more indicative of an emergency than an urgency.
In either circumstance, the complications of hypertensive crisis are
reversible, if the treatment is provided efficiently.3
Any type of
hypertensive disorder may be complicated by the development of hypertensive
crisis. The important proviso is that it is the level of the BP—rather than the
cause of hypertension—that is the main determinant of hypertensive crisis.4
(In select forms of hypertensive crises, however, the rapidity with which the
BP rises seems to be more relevant than the actual level of the BP.) In most
clinical circumstances, immediate BP reduction is indicated, not because of its
absolute level but because the coexisting complications may make any level of
hypertension risky. The risk-benefit ratio of immediate therapy in many forms
of hypertensive crisis is not well-established due to the paucity of controlled
clinical trials.
The most
critical decision in the management of hypertensive emergencies is to assess
the patient's clinical state and to ascertain whether the patient's condition
dictates emergency management. The absolute indications for treatment and
optimal management depend on the underlying and concomitant conditions. A
patient with a true hypertensive crisis should be treated in an ICU.
The choice of
oral versus parenteral drug therapy depends on the urgency of the situation, as
well as on the patient's general condition. The level to which the BP should be
lowered varies with the type of hypertensive crisis and should be individualized.
The choice of parenteral drug is governed by the clinical manifestations and
concomitant medical problems associated with hypertensive crisis. There is no
predetermined level for the goal of therapy.
Complications
of therapy, mainly hypotension and ischemic brain damage, can occur in patients
given multiple potent antihypertensive drugs in large doses without adequate
monitoring.5 Such complications should be minimized by gentle
lowering of BP, careful surveillance, and individualization of therapy.
A relatively
asymptomatic patient who presents with severe hypertension, (a diastolic BP of
130-140 mm Hg), need not be treated with parenteral drugs. These patients
should be managed on an individual basis, and the usual course would be to
intensify or alter the previous antihypertensive therapy.
Once the
hypertensive crisis is resolved and the patient's clinical condition is stable,
the physician should look into factors that might have contributed to the
dangerous elevation of BP (nonadherence to prescribed therapy or the presence
and/or progression of a secondary form of hypertension such as a renal artery
stenosis or renal failure, for example). The physician should discuss
long-range and periodic outpatient follow-up plans with the patient, as close
follow-up is extremely important.
Accelerated and
malignant hypertension Accelerated hypertension is clinically identified by
severe retinopathy (without papilledema), exudates, hemorrhages, arteriolar
narrowing, and spasm. Malignant hypertension is considered a deterioration of
the accelerated form and is distinguished by papilledema. Both the accelerated
and malignant forms of hypertension are associated with severe vascular injury
to the kidney and other target organs. The diagnosis of accelerated or
malignant hypertension is best made clinically on the basis of history and
clinical examination. Simple investigations such as chest radiography, ECG,
urinalysis, and laboratory tests to determine blood count, serum nitrogen
level, creatinine clearance, and electrolyte concentrations are generally sufficient.
The BP level
in malignant hypertension is often quite high, with diastolic levels in the
range of 130 to 140 mm Hg (stage 2 hypertension), but the degree of BP
elevation is an unreliable diagnostic feature (see Table 2). Rather, it is the
degree and extent of vascular injury that determines the clinical
manifestations. Severe headache, with or without coexisting encephalopathy, is
one symptom. Weight loss may occur in some patients with malignant hypertension
as a result of initial natriuresis.
Some patients
with malignant hypertension report visual problems ranging from blurring to
blindness; drowsiness and altered mental status are also common. Worsening
symptoms may indicate progression to encephalopathy or other cerebral
complications, such as stroke. Congestive heart failure can be a feature of
malignant hypertension, either as a consequence of left ventricular
dysfunction, or due to volume retention from concomitant renal failure.
Azotemia, a frequent feature of malignant hypertension, may be associated with
proteinuria. Renal function deteriorates rapidly in many patients without
appropriate therapeutic intervention.
Patients with
accelerated/malignant hypertension should ideally be treated in the hospital,
since the goal of management is not only to lower the BP but to stabilize it,
reverse the target-organ damage, and exclude any reversible causes. Preferably,
these patients should be treated in an ICU; but in the absence of significant
target-organ dysfunction, they can be managed safely on the wards under
supervision.
Although IV
therapy is widely used in the initial treatment of malignant hypertension,
various oral therapies can also be used successfully. ACE inhibitors,
minoxidil, clonidine, prazosin, labetalol, and nifedipine have all been used
for initial treatment of malignant hypertension, but there are no controlled
prospective studies to offer precise guidelines on the preferred therapeutic
options. The choice between oral and parenteral therapy depends on the
monitoring facilities, condition of the patient, and coexisting complications.
Once the BP is brought to safe levels, appropriate oral therapy must be
initiated on the basis of the patient's renal, cardiac, and neurologic status.
Hypertensive encephalopathy is a deadly complication of severe hypertension that
should be recognized as an emergency and quickly treated. Although
encephalopathy occurs mainly in patients with chronic or malignant hypertension,
it can also complicate sudden hypertension of brief duration. The clinical
manifestations are generated not only by the severity of BP elevation but also
by the abrupt rise of BP in a previously normotensive individual. This
condition occurs more frequently when the hypertension is complicated by renal
insufficiency than when the renal function is normal. The full-blown clinical
syndrome of hypertensive encephalopathy may take anywhere from 12 to 48 hours
to develop.
Severe
generalized, sudden headache is a prominent clinical manifestation. Neurogenic
symptoms consisting of confusion, somnolence, and stupor may appear simultaneous
with or following the onset of headache. If untreated, progressive worsening of
neurological damage occurs, culminating in coma and death. The patient may be
restless and uncooperative during the initial stages of the syndrome. Other
clinical features may include projectile vomiting, visual disturbances ranging
from blurring to frank blindness, and transient focal neurologic deficits.
Sometimes (especially in children) generalized or focal seizures may be the
only clinical feature.
On physical
examination of the patient, the BP is markedly elevated but there is no certain
level of BP above which encephalopathy is likely to develop. The fundi reveal
generalized arteriolar spasm with exudates or hemorrhages. Although papilledema
is present in most patients with this complication, its absence does not
exclude the diagnosis of hypertensive encephalopathy.
When a
patient with uncontrolled hypertension presents with severe headache,
fluctuating mental status, papilledema, and variable neurologic deficits, the
most likely initial diagnosis should be hypertensive encephalopathy. This must
be distinguished from other acute neurologic complications of hypertension such
as cerebral infarction or hemorrhage and uremic encephalopathy. A complete but
quick evaluation of the patient should be carried out to consider various
diagnostic possibilities. The only definitive clue to confirm the diagnosis of
hypertensive encephalopathy is the prompt response of the patient's BP
reduction. The syndrome should improve or reverse within a few hours with immediate
control of the hypertension.
Once the
diagnosis of hypertensive encephalopathy is likely, the BP should be lowered
rapidly to near-normal levels; yet the diastolic BP should probably remain at
or slightly above 100 mm Hg. Rapid reduction in the BP produces prompt,
dramatic, and significant relief of the symptoms of hypertensive
encephalopathy. The most important goal of therapy is to prevent permanent
neurologic damage. Although potent orally effective agents like minoxidil and
nifedipine can control severe hypertension, parenteral drugs are preferred in
treating hypertensive encephalopathy successfully.1,6
Severe
hypertension and stroke pose a difficult dilemma. When
intracerebral pressure rises as a result of hemorrhage or thrombotic
infarction, cerebral blood flow may no longer be under normal autoregulation.
Therefore, a reduction in the systemic BP may conceivably compromise the
cerebral flow. Conversely, persistence of severe hypertension may resolve
spontaneously within 48 hours. There are no definitive data in the published
literature that provide the practicing physician with a definitive approach or
guidelines in managing these patients. At times it is difficult to make a
distinction between an ischemic stroke and an intracerebral bleed.
With the
current state of our knowledge, no reliable guidelines can be given for the
management of hypertensive crises occurring in patients with cerebrovascular accidents.
Based on the pathogenesis of these conditions, especially intracerebral
hemorrhage, it is advisable to reduce the BP to near-normal levels or to a
degree that will not clinically compromise cerebral function. If there is
evidence of progression of the disease or worsening of the neurologic
manifestations during treatment, then the therapeutic approach must be
reassessed. Precautions should be taken to avoid hypotension in these patients,
and it is advisable, therefore, not to lower the diastolic BP to less than 100
mm Hg. In any case, the BP reduction should be no more than the approximated
20% of the baseline BP level.
Acute aortic
dissection has severe pain as its cardinal manifestation.7
This pain can easily be confused with the that of
other conditions, such as acute MI. There are certain subtle differences,
however: The pain of dissection is abrupt in onset, severe right from the beginning,
and unremitting in most patients, whereas patients with acute MI rarely report
abrupt onset of pain. The pain of MI may come and go, whereas the pain of
aortic dissection is continuous. Once the diagnosis is suspected, immediate
medical therapy should be implemented pending further diagnostic evaluation.
Two-dimensional
echocardiography, transesophageal echocardiography, CT, tomography,
angiography, and magnetic resonance angiography (MRA) have all been used to
diagnose aortic dissection. MRA combined with transesophageal or transthoracic
echocardiography yields considerable information. However, MRA is recommended
only for patients who are hemodynamically stable. Digital and/or conventional
angiography provides more thorough information concerning the anatomy of
dissection.
Once the
diagnosis of acute aortic dissection is apparent, the following steps should be
undertaken. If the patient is hypertensive, the BP should be reduced to normal
or below-normal levels with drugs that cause the BP to come down smoothly
rather than drastically. Direct vasodilators that reflexively stimulate the
heart should be avoided and they are contraindicated in acute aortic
dissection. When considering medical therapy, keep in mind that the force and
velocity of ventricular contraction (dP/dt) and the pulsatile flow are the
determinants of the shearing force acting on the aortic wall. Attempts should
be made to decrease the dP/dt with a suitable antihypertensive drug.
Pharmacological options for acute aortic dissection include labetalol, a
combined alpha- and beta-blocking drug, and the ultrashort-acting beta-blocker
esmolol, in combination with nitroprusside.
Acute left
ventricular failure may be caused by severe and uncontrolled hypertension; the higher the BP, the harder
the left ventricle must work. Decreasing the workload of the failing myocardium
may improve the heart function. In acute left ventricular failure, myocardial
oxygen requirements increase due to increased end-diastolic fiber length and
left ventricular volume. This could be particularly unfavorable in patients
with concomitant coronary artery disease (CAD).
Prompt
reduction of BP with a balanced vasodilating agent such as nitroprusside is
indicated. Nitroprusside decreases both preload and afterload with restoration
of myocardial function and cardiac output. Although the ACE inhibitors, by the
virtue of their pharmacologic actions, may be useful in this situation, there
is insufficient clinical experience concerning acute therapeutic response to
these agents in patients with left ventricular failure. Morphine, diuretics,
and other standard drugs are also used in this setting.
Severe
hypertension associated with acute ischemic heart disease should benefit from BP reduction in theory, since systemic hypertension
increases myocardial oxygen consumption by increasing the left ventricular wall
tension. But there are no conclusive data to prove that acute treatment is
beneficial. Reduction of systemic BP reduces the cardiac work, wall tension,
and oxygen demand, and may thus limit myocardial necrosis in the early phase of
infarction. With a reduction in the afterload, the hemodynamic status improves
significantly in MI. Carefully supervised treatment of hypertension in patients
with acute MI is, therefore, likely to be beneficial.
Pheochromocytoma
hypertensive crisis may manifest with impressively
dramatic clinical features. The BP is markedly elevated during the paroxysm and
the patient may have profound sweating, marked tachycardia, pallor, numbness,
tingling, and coldness of the feet and hands.8 A
single attack may last from a few minutes to hours and may occur as often as
several times a day to once a month, or less.
If
pheochromocytoma crisis is suspected, the alpha-adrenergic blocking drug
phentolamine (if available) should be given in a dose of 1 to 5 mg IV, to be
repeated within a few minutes if needed. Nitroprusside would be an alternative
to phentolamine, but phentolamine is more specific. A beta-blocking drug may be
useful if the patient has a concomitant cardiac arrhythmia. Administration of
beta-blocking agents should always be preceded by either phentolamine or
pheno-oxybenzamine. Otherwise, beta blockade can aggravate the unopposed
alpha-mediated peripheral vasoconstriction. Labetalol has also been advocated
for this condition, but may not be generally effective in controlling the
clinical manifestations of pheochromocytoma.
Clonidine
withdrawal syndrome can result from abrupt
discontinuation of a high-dosage regimen of clonidine, causing a
hyperadrenergic state that mimics pheochromocytoma. When clonidine is abruptly
discontinued (especially at high dosages) or rapidly tapered, a syndrome
consisting of nausea, palpitation, anxiety, sweating, nervousness, and
headache, along with marked elevation of the BP has been noted. Symptoms of
clonidine withdrawal can be relieved by reinstituting the clonidine regimen. If
there is marked elevation of BP and the patient is experiencing symptoms such
as palpitations, chest discomfort, and epigastric discomfort, the IV
administration of phentolamine or labetalol is recommended.
Monoamine
oxidase inhibitors (MAOIs) can increase the risk of
hypertensive crisis in patients who also take drugs such as ephedrine and
amphetamines or consume foods containing large quantities of tyramine. In the
presence of an inhibitor of monoamine oxidase, tyramine and indirectly acting
sympathetic amines escape oxidative degradation, enter the systemic circulation,
and potentiate the actions of catecholamines. Sympathomimetic amines such as
those contained in nonprescription cold remedies can also provoke this
response. Due to declining use of MAOIs, its reaction is rare.
Cocaine-induced
hypertensive crisis can cause an abrupt, sudden increase
in the systemic BP, resulting in a hypertensive emergency. Neurohumoral factors
triggered by cocaine likely cause intense vasoconstriction and thus increase
the vascular resistance and the BP. Sudden rise of BP in a previously
normotensive individual may result in a serious cardiovascular complication.
The BP should be lowered to safe limits without much delay.
Eclampsia is a potentially serious cardiovascular complication in a pregnant
patient. Although the definitive therapy is delivery of the fetus, the BP
should be reduced to prevent neurologic, cardiac, and renal damage. Although
other antihypertensive drugs may be effective in reducing the BP, the agent of
choice is hydralazine, which has a long record of safety. Animal studies have
shown that nitroprusside can cause problems in the fetus; therefore, its use
should be reserved for hypertension refractory to hydralazine or methyldopa.
The ganglion-blocking drug trimethaphan should be avoided because of the risk
of meconium ileus. In pregnancy-induced hypertension, volume depletion may be
present and diuretics should be avoided. IV labetalol and hydralazine have been
used to treat severe hypertension in pregnancy.9 ACE inhibitors and
angiotensin-receptor blockers should be avoided due to possible fetal/placental
toxicity. Magnesium sulfate is also used as adjunctive therapy to control the
convulsions.
TREATMENT OF
A PATIENT WITH HYPERTENSIVE EMERGENCY
Whether or
not to hospitalize the patient, the therapeutic choices, and the choice of IV
versus oral therapy depend on the clinical evaluation of the patient and
available facilities. Patients with hypertensive emergencies should be
hospitalized, and those with hypertensive urgencies may not always require
admission to the hospital.
The
therapeutic premise underlying the management of hypertensive emergency is not
only to lower the BP quickly but to prevent, arrest, and reverse the target-organ
damage. Therefore, close supervision of the patient is required while the BP is
being lowered. There are no firm guidelines as to the degree of desired BP
reduction, but a reasonable goal for most hypertensive emergencies is to lower
the diastolic BP to 100 mm Hg (or to reduce the mean arterial pressure by 20%)
over a period of minutes to hours.
Hypertensive
emergencies should preferably be managed in an ICU to allow for continuous
monitoring of the general hemodynamic status of the patient. Even though a
secondary form of hypertension, such as renal artery stenosis or adrenal hypertension, may be a causative factor, the immediate goal
should be to lower the BP to a safe level rather than undertaking a diagnostic
workup. The rapidity of onset and duration of action of the chosen drug are
important considerations in treating patients with hypertensive emergencies.
The physician should be familiar with the hemodynamic and pharmacologic actions
of the available drugs.
Role of
concomitant diuretic therapy
Diuretics
have a limited role in the management of hypertensive emergencies; however,
they potentiate the therapeutic response of nondiuretic agents. When the BP
does not respond satisfactorily to an adequate dose of the primary agent,
adding a diuretic (such as furosemide) may be helpful. In volume overload
states such as heart failure, concomitant administration of a loop diuretic is
indicated for optimal results. Diuretics should not be used routinely in the
management of hypertensive crises, as prior volume depletion may be present in
some conditions, such as malignant hypertension. The need for diuretic therapy,
therefore, should be individualized on the basis of the hemodynamic and renal
function status of the patient.
Orally
effective drugs
Clinical
experience has shown that antihypertensive drugs given orally as either single
or multiple doses can lower the BP immediately in patients with severe
hypertension. Obviously, this therapeutic opportunity is most suitable for
patients with hypertensive urgencies, not emergencies.
Nifedipine, a calcium channel blocker given either orally or
sublingually, has been shown to lower the BP rapidly and can be useful
in the management of hypertensive crisis. Immediate reduction in BP can be
accomplished with sublingual (a punctured capsule, or nifedipine liquid drawn
out of the capsule with a syringe) or oral administration of the capsules. The
drug is also effective when the capsule is bitten and then swallowed. The
advantages of nifedipine are rapid onset of action and lack of CNS depression.
It may cause reflex tachycardia. As the duration of action of nifedipine is
short, patients who receive this drug for hypertensive emergencies should be
monitored for several hours to consider re-administration of the drug. An
abrupt fall in the BP induced by nifedipine administration can cause certain
adverse effects—symptomatic hypotension, tachycardia, and ischemic events—so
the clinical need to use nifedipine capsules to lower the BP urgently should be
carefully assessed and avoided, if possible.
Clonidine has been shown to produce an immediate antihypertensive effect when
given in repetitive doses. Typically, clonidine loading was accomplished in the
ED by administering it orally at a dosage of 0.1 mg q1h until the desired goal
was obtained. The use of clonidine loading therapy has declined due to the
availability of safer and better-tolerated alternative therapies that do not
cause drowsiness.
Captopril is an ACE inhibitor that has been found to be effective in the immediate
treatment of severe hypertension and hypertensive crises. Captopril lowers the
BP promptly without causing tachycardia, and thus offers a distinct hemodynamic
advantage over direct arteriolar dilators. The maximal effect from orally
administered captopril may not be attained for as long as 2 hours. There are
some reports documenting the effectiveness of sublingual captopril in the
treatment of hypertensive crisis, but further data needs to be generated to
define its role in the acute management of hypertensive crisis.
Minoxidil, a powerful direct vasodilator, has been successfully used in the
treatment of refractory or severe hypertension. Because of its relatively rapid
onset of action and sustained duration, this drug has been used for the
treatment of hypertensive crises. Minoxidil in dosages ranging from 2.5 to 10
mg can be given every 4 to 6 hours initially in the treatment of severe
hypertension. It works best when given along with a diuretic, and an adrenergic
blocker is necessary to counteract the reflex tachycardia. Minoxidil should be
used with caution in patients with acute coronary syndromes unless the patient
is beta-blocked.
Labetalol can be administered orally in doses of 100 to 300 mg for the treatment of
hypertensive urgencies. Because of its dual adrenergic blockade, the fall in BP
is not accompanied by reflex tachycardia. This attribute can be especially
beneficial in patients with CAD. Oral labetalol is effective within 1 to 3
hours and may be useful for hypertensive urgencies, but it has an unpredictable
dose response and thus may not be ideal for acute situations. Labetalol is
contraindicated in patients with bronchospasm, heart block, significant
bradycardia or heart failure.
IV drugs for
hypertensive emergencies Several IV drugs are effective for use in hypertensive
crisis. The patient's clinical presentation will determine the agent of choice
in an individual situation. Parenteral drugs for rapid control of severe
hypertension are shown in Table 3.
Nitroprusside is a powerful BP-lowering drug that possesses the properties of rapid
onset and offset of action. The hypotensive response occurs within seconds
after the infusion is started and disappears almost as rapidly when the
infusion is discontinued. The initial infusion rate should be 0.3 mcg/kg/min, which can be increased every 5 minutes until a
desired BP level is obtained. Once the desired effect is achieved, the
BP should be continuously monitored. Hypotension is the most common—but
avoidable—adverse effect of nitroprusside therapy. Cyanide toxicity from
nitroprusside is possible, although extremely rare. Prophylactic infusion of
cyanocobalamin (vitamin B12a) 25 mg/h, has been shown to decrease
the cyanide concentration and tissue hypoxia resulting from nitroprusside
infusion during surgery. Thiocyanate toxicity secondary to nitroprusside is
uncommon and occurs only with high doses and in the presence of renal failure.
Treatment should be interrupted when the thiocyanate level is close to 10
mg/dL. Monitoring of plasma thiocyanate levels is not mandatory, as long as the
patient's clinical status is closely assessed. Treatment of suspected
thiocyanate toxicity requires discontinuation of the drug and institution of
dialysis.
Labetalol can be used parenterally or orally for the treatment of hypertensive
emergencies. IV labetalol administered as either a continuous infusion or as
bolus injections reduces the BP promptly because of its rapid onset of action.
Controlled smooth reduction in BP may be obtained by continuous infusion of
labetalol at the rate of 0.5 to 2 mg/min. As with nitroprusside, close
monitoring of the patient is required during the infusion of labetalol. Rapid
(but not abrupt) lowering of BP can also be accomplished with bolus injections
of labetalol. Labetalol should not be used when beta-blockers are
contraindicated—for example, in patients who may have heart failure,
atrioventricular block, asthma, or chronic obstructive pulmonary disease.
Nicardipine is a dihydropyridine calcium antagonist that exerts a prompt hemodynamic
effect when given IV in patients with severe hypertension. Nicardipine infusion
is started at 5 mg/h, and can be titrated upwards gradually to obtain the
desired therapeutic effect.11 Once a stable
BP is reached, most patients do not require further dosage alterations. Thus,
nicardipine pharmacodynamics resemble those of
nitroprusside in terms of the onset, and duration and offset of action. Because
of its mechanism of action (calcium channel blockade), nicardipine may be
beneficial in preserving tissue perfusion. It is a good option in the
management of severe hypertension with or without target-organ damage.
Hydralazine has an antihypertensive action that results from a direct relaxation of
the vascular smooth muscle and it is accompanied by reflex increases in stroke
volume and heart rate, which can precipitate myocardial ischemia. Either IM or
IV administration of hydralazine causes an unpredictable but definite fall in
BP. In the treatment of hypertensive emergencies, the initial IV dose should be
10 to 20 mg. The onset of the hypotensive effect occurs within 10 to 30
minutes, and its duration of action ranges from 3 to 9 hours. The dose and
frequency of administration necessary to control the BP are highly variable.
The delayed onset and unpredictable degree of hypotensive effect present
difficulties in titration. Nevertheless, hydralazine continues to be
successfully utilized in the treatment of eclampsia.
Phentolamine is an alpha receptor-blocking agent that is specifically indicated for
treating hypertensive crises associated with increased circulating
catecholamines. These include, for example, pheochromocytoma crisis, certain
cases of clonidine withdrawal syndrome, and crises resulting from an MAOI and
drug-food interaction. The hypotensive effect of a single bolus injection is
short-lived and lasts less than 15 minutes. This drug may precipitate angina or
cardiac arrhythmias.
Nitroglycerin is a weak systemic arterial dilator with a greater effect on large
arteries than on smaller arteries. Low doses cause venodilation; much higher
doses are required to produce a fall in systemic BP. Because of its
pharmacologic actions, nitroglycerin infusion may be particularly beneficial in
patients with CAD either with or without hypertension. Nitroglycerin improves
coronary perfusion. Although there are no controlled studies, nitroglycerin
therapy can be considered in the management of severe hypertension associated
with CAD. The usual initial dosage of nitroglycerin is 5 to
15 mcg/min, and the dosage is titrated upward to a desired therapeutic
end point. It has a rapid onset (2-5 minutes) and offset of action. Although
nitroglycerin has been used to achieve controlled hypotension, its main use
continues to be in patients with unstable angina and acute MI. Prolonged use
may result in tolerance. Isosorbide dinitrate therapy has also been utilized
for immediate treatment of severe hypertension but its precise role and
guidelines on how to use it are not fully delineated.12
Enalaprilat, by its mechanism of action, prevents conversion of angiotensin I to
angiotensin II by blocking angiotensin converting enzyme and thus lowering BP.
Enalaprilat is the only available parenteral ACE inhibitor. For hypertensive
emergencies, it is given at a dosage of 0.625 to 1.25 mg IV over 5 minutes and
may be repeated every 6 hours. ACE inhibitors are contraindicated in patients
with renal artery stenosis and in pregnant patients. ACE inhibitors can cause
precipitous falls in BP in patients who are hypovolemic. These drugs are
especially valuable in treating hypertensive emergencies in patients with
chronic heart failure.
Fenoldopam is a relatively new drug that is a selective dopamine (DA1)
receptor agonist and causes significant vasodilation. It is a short-acting,
parenteral arteriolar vasodilator that lowers BP by reducing peripheral
vascular resistance.13,14 By the mode of
its action on the DA1 receptor, fenoldopam causes remarkable renal
vasodilation and promotes diuresis and natriuresis. The half-life of fenoldopam
is estimated to be 5 minutes, and the recommended starting dosage is 0.1 mcg/
kg/min. Its onset of action is 5 minutes and maximum response is achieved
within 15 minutes. The dosage should be titrated to gradually attain the goal
BP. It can lower BP in hypertensive emergencies safely and effectively and at
the same time preserve or improve renal blood flow and cause diuresis and
natriuresis. Therefore, it may offer important advantages. A number of early
comparative studies between nitroprusside and fenoldopam showed that while both
are equally effective in reducing the BP, fenoldopam offers important renal
advantages over nitroprusside.
References
1. Burt VL, Cutler JA, Higgins M, et al.
Trends in the prevalence, awareness, treatment and control of hypertension in
the adult US population: data from the health examination surveys, 1960 to
1991. Hypertension 1995;26:60-69. [Erratum,
Hypertension 1996;27:1192.] [Free Full Text]
2. The sixth report of the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1997;157:2413-2446. [Erratum, Arch Intern
Med 1998;158:573.] [Abstract]
3. Forette F, Seux
ML, Staessen JA, et al. Prevention of
dementia in randomised double-blind placebo-controlled Systolic Hypertension in
Europe (Syst-Eur) trial. Lancet 1998;352:1347-1351. [CrossRef][ISI][Medline]
4. Kannel WB. Elevated systolic blood
pressure as a cardiovascular risk factor. Am J Cardiology 2000;15:251-5.
5. Staessen JA, Gasowski J, Wang JG, et al. Risks of
untreated and treated isolated systolic hypertension in the elderly:
meta-analysis of outcome trials. Lancet 2000;355:865-872.
[Erratum, Lancet 2001;357:724.] [CrossRef][ISI][Medline]
6. Stamler J. Blood pressure and high blood pressure:
aspects of risk. Hypertension 1991;18:Suppl I:I-95.
7. Perloff D,
Grim CM, Flack J, et al. Human blood pressure determination by
sphygmomanometry. Circulation 1993;88:2460-2470. [Free Full Text]
8. Pickering TG. Recommendations for the
use of home (self) and ambulatory blood pressure monitoring. Am J
Hypertens 1996;9:1-11. [CrossRef][ISI][Medline]
9. Kannel WB. Potency of vascular risk
factors as the basis for antihypertensive therapy. Eur Heart J
1992;13:Suppl G:34-42.
10. Dustan HP, Schneckloth RE, Corcoran AC, Page IH. The effectiveness of long-term treatment of malignant hypertension.
Circulation 1958;18:644-651. [Free Full Text]
11. Collins R,
Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary disease. 2.
Short-term reductions in blood pressure: overview of randomized drug trials in
their epidemiological context. Lancet 1990;335:827-838. [CrossRef][ISI][Medline]
12. Psaty BM, Smith NL, Siscovick DS, et
al. Health outcomes associated with antihypertensive therapies used as
first-line agents: a systematic review and meta-analysis. JAMA 1997;277:739-745. [Abstract]
13. Appel LJ, Moore TJ, Obarzanek E, et
al. A clinical
trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-1124. [Free Full Text]
14. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on
blood pressure of reduced dietary sodium and the Dietary Approaches to Stop
Hypertension (DASH) diet. N Engl J Med 2001;344:3-10. [Free Full Text]
15. Midgley JP,
Matthew AG, Greenwood CM, Logan AG. Effect of reduced dietary sodium on blood
pressure: a meta-analysis of randomized controlled trials. JAMA
1996;275:1590-1597. [Abstract]
16. Cutler JA, Follmann D, Allender PS. Randomized
trials of sodium reduction: an overview. Am J Clin Nutr 1997;65:Suppl:643S-651S. [Abstract]
17. Alderman MH,
Madhavan S, Cohen H. Low urinary sodium is associated with greater risk of
myocardial infarction among treated hypertensive men. Hypertension 1995;25:1144-1152. [Free Full Text]
18. Kumanyika SK,
Cutler JA. Dietary sodium reduction: is there cause for concern? J Am Coll
Nutr 1997;16:192-203. [Abstract]
19. Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S,
Lacy CR. Effects of reduced sodium intake on hypertension control in older
individuals: results from the Trial of Nonpharmacologic Interventions in the
Elderly (TONE). Arch Intern Med 2001;161:685-693. [Free Full Text]
20. Neaton JD, Grimm RHJ, Prineas RJ, et al. Treatment of
Mild Hypertension Study: final results. JAMA 1993;270:713-724. [Abstract]
21. Grimm RH Jr, Grandits GA, Cutler JA, et al.
Relationships of quality-of-life measures to long-term lifestyle and drug
treatment in the Treatment of Mild Hypertension Study. Arch Intern Med 1997;157:638-648. [Abstract]
22. Hansson L, Zanchetti A, Carruthers
SG, et al. Effects of intensive blood-pressure lowering and low-dose
aspirin in patients with hypertension: principal results of the Hypertension
Optimal Treatment (HOT) randomized trial. Lancet 1998;351:1755-1762. [CrossRef][ISI][Medline]
23. UK Prospective Diabetes Study Group. Tight blood pressure
control and risk of macrovascular and microvascular complications in type 2
diabetes: UKPDS 38. BMJ 1998;317:703-713. [Erratum, BMJ 1999;318:29.] [Free Full Text]
24. SHEP
Cooperative Research Group. Prevention of stroke by antihypertensive drug
treatment in older persons with isolated systolic hypertension: final results
of the Systolic Hypertension in the Elderly Program (SHEP). JAMA 1991;265:3255-3264. [Abstract]
25. Materson BJ, Reda DJ, Cushman WC, et al. Single-drug
therapy for hypertension in men: a comparison of six antihypertensive agents
with placebo. N Engl J Med 1993;328:914-921. [Erratum,
N Engl J Med 1994;330:1689.] [Free Full Text]
26. Blood
Pressure Lowering Treatment Trialists' Collaboration. Effects of ACE
inhibitors, calcium antagonists, and other blood-pressure-lowering drugs:
results of prospectively designed overviews of randomised trials. Lancet
2000;356:1955-1964. [CrossRef][ISI][Medline]
27. The Heart Outcomes Prevention
Evaluation Study Investigators. Effects of an
angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in
high-risk patients. N Engl J Med 2000;342:145-153.
[Erratum, N Engl J Med 2000;342:748, 1376.] [Free Full Text]
28. Staessen JA,
Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a
meta-analysis. Lancet 2001;358:1305-1315. [Erratum, Lancet 2002;359:360.] [CrossRef][ISI][Medline]
29. Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford
N, Schrier RW. The effect of nisoldipine as compared with
enalapril on cardiovascular outcomes in patients with non-insulin-dependent
diabetes and hypertension. N Engl J Med 1998;338:645-652. [Free Full Text]
30. Hansson L,
Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive
drugs in elderly patients: cardiovascular mortality and morbidity the Swedish
Trial in Old Patients with Hypertension-2 study. Lancet
1999;354:1751-1756. [CrossRef][ISI][Medline]
31. Dahlof B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan
Intervention For Endpoint reduction in hypertension
study (LIFE): a randomised trial against atenolol. Lancet 2002;359:995-1003. [CrossRef][ISI][Medline]
32. Pahor M, Psaty BM, Alderman MH, et
al. Health outcomes associated with calcium antagonists compared with other
first-line antihypertensive therapies: a meta-analysis of randomised controlled
trials. Lancet 2000;356:1949-1954. [CrossRef][ISI][Medline]
33. Major outcomes in high-risk hypertensive patients
randomized to angiotensin-converting enzyme inhibitor or calcium channel
blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to
Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981-2997. [Free Full Text]
34. Wing LMH,
Reid CM, Ryan P, et al. A comparison of outcomes with angiotensin-converting-enzyme
inhibitors and diuretics for the treatment of hypertension in the elderly.
N
Engl J Med 2003;348:583-592. [Free Full Text]
35. Lewis EJ, Hunsicker LG, Bain RP,
Rhode RD. The effect of
angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl
J Med 1993;329:1456-1462. [Erratum, N Engl J Med 1993;330:152.] [Free Full Text]
36. Hostetter TH.
Prevention of end-stage renal disease due to type 2 diabetes.
N Engl J Med 2001;345:910-912. [Free Full Text]
37. Furberg CD, Psaty BM. Should calcium antagonists be first-line agents in the treatment of cardiovascular
disease? The public health perspective. Cardiovasc
Drugs Ther 1996;10:463-466. [ISI][Medline]
38. Saunders E, Weir MR, Kong BW, et al. A comparison of the efficacy and safety of a B-blocker, a
calcium-channel blocker, and a converting enzyme inhibitor in hypertensive
blacks. Arch Intern Med 1990;150:1707-1713. [Abstract]
39. Neutel JM, Smith DHG, Weber MA. Low dose combination therapy vs.
high dose monotherapy in the management of hypertension. J Clin
Hypertens (Greenwich) 1999;1:79-86.
40. Prisant LM, Weir MR, Papademetriou V,
et al. Low-dose drug combination therapy: an
alternative first-line approach to hypertension treatment. Am Heart J
1995;130:359-366. [ISI][Medline]
41. Guidelines Subcommittee of the World Health
Organization-International Society of Hypertension (WHO-ISH). 1999 World Health Organization-International Society of Hypertension
Guidelines for the Management of Hypertension. J Hypertens
1999;17:151-183. [CrossRef][ISI][Medline]
42. Ramsay LE, Williams B, Johnston GD,
et al. British Hypertension Society guidelines for hypertension management
1999: summary. BMJ 1999;319:630-635. [Free Full Text]
43. Jackson R, Barham P, Bills J, et al. Management of
raised blood pressure in New Zealand. BMJ 1993;307:107-110. [ISI][Medline]
44. Hoes AW, Grobbee DE, Lubsen J. Does drug treatment improve
survival? Reconciling the trials in mild-to-moderate
hypertension. J Hypertens 1995;13:805-811. [ISI][Medline]
45. Vasan RS, Larson MG, Leip EP, et al.
Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001;345:1291-1297. [Free Full Text]
46. Mann SJ, Blumenfeld JD, Laragh JH. Issues, goals, and guidelines for
choosing first-line and combination antihypertensive drug therapy. In: Laragh JH, Brenner BM, eds. Hypertension:
pathophysiology, diagnosis, and management, 2nd ed. Vol. 2. New York: Raven
Press, 1995:2531-42.
![]() 140 mm Hg or
diastolic pressure
140 mm Hg or
diastolic pressure ![]() 90 mm Hg) is present in one in four adults in the United
States.1 The prevalence is higher among blacks
and older persons, especially older women. Table 1 shows the classification of
blood pressure according to the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.2 Hypertension is a risk
factor for stroke, myocardial infarction, renal failure, congestive
heart failure, progressive atherosclerosis, and dementia.3 Systolic pressure
is a stronger predictor of
cardiovascular events than is diastolic pressure,4 and isolated systolic hypertension, which
is common among older persons, is particularly hazardous.5 There is a continuous, graded relation between blood
pressure and the risk of
cardiovascular disease; the level and duration of hypertension and the presence or absence of coexisting cardiovascular risk
factors determine the outcome.6 Treatment of hypertension reduces the risk of stroke, coronary artery disease, and congestive
heart failure, as well as overall cardiovascular morbidity and mortality
from cardiovascular causes. However, only 54 percent of patients with hypertension receive treatment and only 28 percent
have adequately controlled blood pressure.1
90 mm Hg) is present in one in four adults in the United
States.1 The prevalence is higher among blacks
and older persons, especially older women. Table 1 shows the classification of
blood pressure according to the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.2 Hypertension is a risk
factor for stroke, myocardial infarction, renal failure, congestive
heart failure, progressive atherosclerosis, and dementia.3 Systolic pressure
is a stronger predictor of
cardiovascular events than is diastolic pressure,4 and isolated systolic hypertension, which
is common among older persons, is particularly hazardous.5 There is a continuous, graded relation between blood
pressure and the risk of
cardiovascular disease; the level and duration of hypertension and the presence or absence of coexisting cardiovascular risk
factors determine the outcome.6 Treatment of hypertension reduces the risk of stroke, coronary artery disease, and congestive
heart failure, as well as overall cardiovascular morbidity and mortality
from cardiovascular causes. However, only 54 percent of patients with hypertension receive treatment and only 28 percent
have adequately controlled blood pressure.1 





 Some patients who have what appears to be resistant hypertension
have a normal blood pressure at home. This phenomenon has been attributed
to transitory, or "white-coat," resistant hypertension
in the physician's office. Repeated home measurements or 24-hour ambulatory
monitoring may differentiate this type of hypertension from
truly resistant hypertension.13 Such measures are warranted in patients undergoing treatment
who have consistently high blood-pressure levels in the physician's
office yet have no evidence of target-organ damage. In one study, as
many as a third of patients with apparently resistant
hypertension had average blood-pressure levels of
less than 130/85 mm Hg on 24-hour or home measurement.14 Some data suggest that blood-pressure values obtained at
home or during 24-hour ambulatory procedures correlate better with
target-organ involvement, especially left ventricular hypertrophy,
than do values obtained in the physician's office.15 However, office, or white-coat, hypertension is not
benign and should not be ignored.
Some patients who have what appears to be resistant hypertension
have a normal blood pressure at home. This phenomenon has been attributed
to transitory, or "white-coat," resistant hypertension
in the physician's office. Repeated home measurements or 24-hour ambulatory
monitoring may differentiate this type of hypertension from
truly resistant hypertension.13 Such measures are warranted in patients undergoing treatment
who have consistently high blood-pressure levels in the physician's
office yet have no evidence of target-organ damage. In one study, as
many as a third of patients with apparently resistant
hypertension had average blood-pressure levels of
less than 130/85 mm Hg on 24-hour or home measurement.14 Some data suggest that blood-pressure values obtained at
home or during 24-hour ambulatory procedures correlate better with
target-organ involvement, especially left ventricular hypertrophy,
than do values obtained in the physician's office.15 However, office, or white-coat, hypertension is not
benign and should not be ignored. 
![]() 2-adrenergic blockers, reserpine (in low doses), and direct
vasodilators (hydralazine or, in rare cases, minoxidil) — may be necessary
in some cases, as tolerated. With direct vasodilators, concomitant
high-dose beta-blockers (metoprolol or atenolol) and loop diuretics
(furosemide) will be needed to counteract reflex tachycardia and
edema. Aside from the aldosterone antagonist spironolactone and
alpha-blockers, which have been shown to reduce blood pressure in
patients with resistant
hypertension, data are
lacking to predict the magnitude of further blood-pressure reduction
associated with the addition of one of these other medications;
clinical experience suggests a decrease in systolic pressure of
about 5 to
2-adrenergic blockers, reserpine (in low doses), and direct
vasodilators (hydralazine or, in rare cases, minoxidil) — may be necessary
in some cases, as tolerated. With direct vasodilators, concomitant
high-dose beta-blockers (metoprolol or atenolol) and loop diuretics
(furosemide) will be needed to counteract reflex tachycardia and
edema. Aside from the aldosterone antagonist spironolactone and
alpha-blockers, which have been shown to reduce blood pressure in
patients with resistant
hypertension, data are
lacking to predict the magnitude of further blood-pressure reduction
associated with the addition of one of these other medications;
clinical experience suggests a decrease in systolic pressure of
about 5 to